Abstract
Objective
Telerehabilitation for individuals with vision impairment aims to maintain maximum physical and/or psychological functioning through remote service delivery. This review aims to describe the type of telerehabilitation services available to people with vision impairment and summarise evidence on health-related outcomes, well-being and cost-effectiveness.
Design
Scoping review.
Data sources
CINAHL Plus, MEDLINE, PsycARTICLES, PsychINFO, Embase, PubMed, HMIC and Ovid Emcare were searched, without date restrictions up to 24 May 2021. Charity and government websites, conference proceedings and clinical trial databases were also examined.
Eligibility criteria
Eligible studies evaluated benefits of telerehabilitation services for adults with vision impairment. Studies were excluded if they were not available in English, or focused on distance learning of visually impaired students.
Data extraction and synthesis
Two independent reviewers screened articles and extracted data. A risk of bias analysis was performed.
Outcome measures
Measures of benefit included performance-based assessment, patient-reported outcomes and cost-effectiveness.
Results
Of 4472 articles, 10 eligible studies were included. Outcomes addressed patient satisfaction (n=4;33.3%), quality-of-life, activities of daily living and well-being (n=4;33.3%), objective visual function (n=2;16.6%) and knowledge relating to ocular symptoms (n=1;8.3%). Two studies addressed multiple outcomes. Cost-effectiveness was addressed in one article (8.3%). Patients were generally satisfied with their experiences, which had a range of positive benefits on functional and quality-of-life outcomes in areas relating to daily activities (eg, reading, making phone calls). Telerehabilitation allowed patients to undertake vision optimisation training to prevent vision deterioration. Grey literature indicated that there are no completed clinical trials relating to low vision telerehabilitation. Charity services had implemented digital skills training to help beneficiaries communicate remotely.
Conclusion
While acceptability of telerehabilitation was mostly high, limited real-world data are available which raises questions around the long-term desirability of this approach. Further trials are needed to evaluate telerehabilitation using a robust set of outcome measures.
PROSPERO registration number
CRD42021254825.
Keywords: ophthalmology, rehabilitation medicine, quality in health care
Strengths and limitations of this study.
This review provides novel findings informing design of future trials and evaluations of telerehabilitation.
Inclusion of grey literature reduces publication bias and increases the comprehensiveness of the review.
Only articles written in English were included and results were seldom disaggregated by disease type or severity.
Introduction
Visual impairment is a broad term used to describe a reduction in visual sensitivity that cannot be corrected by standard eyeglasses or medical treatment. It is estimated that over 2 million people in the UK are living with a form of visual impairment.1 People with visual impairment may be classified as ‘sight impaired’ (ie, partially sighted) or ‘severely sight impaired’ (ie, legally blind).2 The impact of visual impairment can be complex and highly heterogenous, affecting aspects of daily functioning, mobility and quality of life.3–8 Among the widely prevalent ophthalmic conditions such as age-related macular degeneration, glaucoma and diabetic retinopathy, sight loss is typically progressive and irreversible; hence, support relies heavily on rehabilitation to promote adaption, enabling patients to better manage the challenges associated with vision loss and to live an independent and fulfilling life.9 10
The mainstay of rehabilitation is to restore or maintain physical and/or psychological functioning to the maximum degree possible in individuals living with disease or injury.11 In vision rehabilitation, eye care providers are encouraged to provide rehabilitative support or refer patients to relevant services, even in cases of mild or moderate sight loss.12 Rehabilitation encompasses many disciplines, and interventions may include provision of visual aids, devices and software, behavioural training, home environment assessments and adaptions, social and psychological support, leisure and vocational activities or a combination of these strategies.13 14 However, rehabilitation is characteristically structured around overcoming the practical and functional challenges of sight loss, while psychological outcomes are seldom addressed directly.15 The type of services which are offered often depends on the nature of the visual impairment. For example, the rehabilitative needs of individuals with central visual field loss may differ from those with impaired peripheral vision.16 The traditional mode of delivery for vision rehabilitation has been in face-to-face settings within outpatient clinics or home visits by low vision specialists or allied health professionals; though digital developments have increased opportunity for remote service delivery (ie, telerehabilitation).
Telerehabilitation, also known as virtual training, refers to delivering rehabilitative services using a remote or virtual approach, facilitated by telecommunication technologies. Services may comprise a range of elements designed to assess, prevent, treat, educate or counsel individuals living with chronic health conditions.17 Telerehabilitation services may be synchronous, whereby services are delivered in real-time using two-way video or audio communication, or asynchronous, such as remote evaluation of recorded videos or other measurements such as surveys or psychophysical testing.18 Compared with traditional face-to-face rehabilitation, telerehabilitation offers potential benefits, such as reduced costs, increased geographical accessibility and creating opportunities to extend limited resources.19 Moreover, telerehabilitation has been identified as an effective means of delivering support to individuals with chronic conditions including multiple sclerosis, osteoarthritis and stroke.20–22
While there is convincing evidence to suggest telerehabilitation can be effective at improving physical and psychological functioning in people living with chronic health conditions,20–22 less is known about the benefits of telerehabilitation services for people with a vision impairment. For example, a previous systematic review sought to compare outcomes between face-to-face and virtual vision rehabilitation services, yet no completed studies were found.23 Additionally, new services such as remote delivery of clinical care (telehealth) are likely to have emerged during the COVID-19 pandemic which have yet to be reviewed. This is significant given the rapid and extensive scale-up of telehealth services since the beginning of the pandemic.24 25 This scoping review, therefore, aims to draw together evidence on telerehabilitation services, and describe their impact on health and well-being outcomes in people with vision impairment.
Objectives
Describe the type of telerehabilitation services available to people with visual impairment.
Provide insight on the impact of telerehabilitation in terms of health-related outcomes, well-being and cost-effectiveness.
Methods
This review follows best practice for conducting scoping reviews as outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for Scoping Reviews checklist to ensure all aspects of the process are undertaken using rigorous and transparent methods.26 A search of the electronic databases CINAHL Plus and MEDLINE (via EBSCOhost) and PsycARTICLES, PsycINFO, Embase, PubMed, HMIC and Ovid Emcare (via Ovid) was undertaken without date restrictions or topic filters. As recommended by The Cochrane Handbook for Systematic Reviews of Interventions, medical subject headings (MeSH) were used to identify the most relevant articles.27 MeSH terms are official words or phrases selected to represent medical concepts and are assigned to articles in order to describe what the research item is about.28 This process provided a list of keywords relating to vision impairment and telerehabilitation. For detailed search terms, see table 1. Reference lists of included studies and any identified systematic reviews were also reviewed for relevant articles, and citation tracking was performed using Google Scholar.
Table 1.
Search terms
| Vision impairment term | Telerehabilitation term | |
| vision OR low vision OR vision loss OR reduced vision OR subnormal vision OR diminished vision OR vis* impair* OR sight loss OR blind* OR partially sighted | AND | telerehab* OR tele-rehab* OR remote rehab* OR virtual rehab* OR e-learning OR online learning OR online training OR telephone training OR telephone rehab* OR telephone learning OR virtual learning OR web training OR virtual training |
In addition, we reviewed online conference proceedings for relevant abstracts by searching the websites of the International Society of Physical and Rehabilitation Medicine; American Congress of Rehabilitation Medicine; Association for Research in Vision and Ophthalmology; American Academy of Ophthalmology; European Association for Vision and Eye Research. A search of grey literature included searching for relevant articles or reports on the websites of organisations such as the UK National Institute for Health and Clinical Excellence (www.nice.org.uk) and National Health Service Evidence (www.evidence.nhs.uk). WHO International Clinical Trials Registry Platform and the US National Institute of Health trial register (ClinicalTrials.gov) were searched for ongoing and completed trials relating to vision impairment and telerehabilitation. We also conducted an extensive search of the UK Charity Commission website to identify organisations with links to vision impairment and rehabilitation. Relevant charity websites were then searched and in cases where telerehabilitation was documented, any available documentation was downloaded and reviewed, and charities were contacted to enquire about the current status of telerehabilitation.
Population
Adult patients (aged 18 years or older) with visual impairment caused by any underlying condition, medical or non-medical trauma.
Intervention
The scoping review considered how telerehabilitation services have impacted people with vision impairment. Where available, evidence on cost-effectiveness will be included. The review included studies where a telerehabilitation service is delivered and evaluated, which could relate to improving well-being; increased social participation/connectivity; maintaining activities of daily living (eg, mobility); optimisation of vision.
Articles written in English, with no restrictions on publication period, and only where the full text was available were included. Studies were required to address the intervention (telerehabilitation) and population of interest (adults with visual impairment). Articles were excluded if they did not relate to remote service delivery (ie, face-to-face services). Articles focusing only on an educational context (eg, e-learning) were also excluded. For example, visually impaired students using home technology for distance learning.
Two authors (LJ and ML) independently screened studies using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org) to assess eligibility. Any disagreement in coding decisions were resolved through discussion. Relevant information (eg, publication details, characteristics of participants, study design, outcomes measured, study results and conclusions) from eligible articles was entered into a data extraction table.
Studies were assessed for quality using Kmet et al. ‘Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields’.29 This quality appraisal tool was chosen because of both quantitative and qualitative studies emerging from the literature search. The tool uses a checklist to provide guidance on study aspects which should be considered when making a decision regarding quality of reporting. For example, in response to the item regarding subject characteristics, the study in question must provide at least the age and sex of participants. This review is registered online with the International prospective register of systematic reviews (PROSPERO; www.crd.york.ac.uk/prospero/; Reference CRD42021254825).
Patient and public involvement
No patients were involved in the design of the review. We will disseminate plain language summaries to relevant patient groups including beneficiaries of Blind Veterans UK.
Results
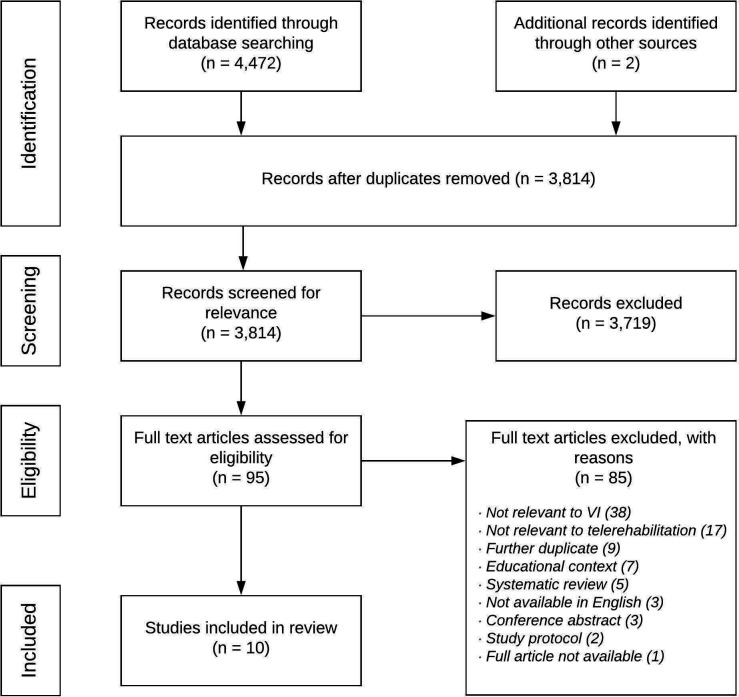
Searches were run on 24 May 2021 and yielded 4472 results. Of these, 658 were automatically removed as duplicates. This left 3814 studies to screen using title and abstract, of which 3719 were excluded and 95 were assessed for full-text eligibility. Studies were mostly excluded at the title and abstract screening stage because they did not relate to telerehabilitation or did not involve people with a vision impairment. These two reasons were also the primary cause for exclusion in the full-text review accounting for 17 and 38 exclusions, respectively. A further two studies were added through reference list searching. Ultimately, 10 full-text studies were selected for inclusion. The study selection process is shown in the PRISMA diagram in figure 1.
Figure 1.
PRISMA diagram showing study selection process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; VI, vision impairment.
Two authors (LJ and ML) independently assessed the quality of all 10 studies. The lowest score was 0.64, the highest was 1.00 (ie, all responses to relevant questions in the Kmet et al appraisal criteria were ‘Yes’), and the median score was 0.93. Full details of quality appraisal are provided in online supplemental material 1.
bmjopen-2021-059985supp001.pdf (63.3KB, pdf)
The following overview of study findings is organised according to the main outcome domains for each of the 10 articles identified in the literature search. Two articles feature in more than one section as the outcomes were translatable across multiple domains. Four studies (33.3%) addressed patient satisfaction,30–33 two studies (16.6%) related to objective visual function,34 35 four studies (33.3%) measured patient-reported outcomes, activities of daily living and well-being,33 34 36 37 one study (8.3%) addressed knowledge relating to ocular symptoms,38 and a further one study (8.3%) was an analysis of cost-effectiveness.39 Six studies used a synchronous modality whereas four studies were asynchronous in nature. For full details of the included studies, refer to the data extraction table (online supplemental material 2).
bmjopen-2021-059985supp002.pdf (74.8KB, pdf)
Patient satisfaction
Four articles explored patients’ satisfaction with telerehabilitation which led to recommendations for key features to improve uptake of services. Three of these articles reported the findings of feasibility studies,31–33 and one was a qualitative analysis of patient experiences.30 All of these studies included participants with a visual impairment caused by a range of pathologies including age-related macular degeneration, optic nerve disease, retinitis pigmentosa, and stroke-related visual field deficit.
Dunne et al’s30 study of stroke survivors reports the outcomes of qualitative interviews and focus groups with patients and carers. The study was informed by the findings of a survey of Stroke Association group members in the UK and the aims were to understand experiences of using a compensatory eye-movement tool and training packages. The Durham Reading and Exploration Training (DREX) is a computer-based telerehabilitation system teaching adaptive eye movement strategies to enable stroke survivors to cope more effectively with visual field deficits.40 DREX is a mobile application which incorporates tasks that combine both reading and exploration (eg, scanning an array to locate a target). In the context of rehabilitation, the application is asynchronous in nature whereby healthcare professionals can access and review patients’ results at a later time through a clinical portal. The wider study required patients with stroke-related visual field defects to complete the DREX trials on a tablet in their own homes and outcomes were compared with a control intervention, which consisted of attention-based tasks with no eye movement or exploration exercises. Significantly greater gains were observed in visual exploration (12.9%, 95% CI 8.4% to 17.3%) and reading (18.5%, 95% CI 9.9% to 27.0%) following DREX than in the control intervention for both tasks, respectively (exploration=4.8%, 95% CI 0.1% to 9.5%; reading=1.6%, 95% CI −4.8% to 8.7%).40 Qualitative responses highlighted a range of issues in the application of telerehabilitation for visually impaired stroke survivors. For example, a lack of confidence with technology, perceived fear of making mistakes while online, distrust of the quality of the intervention, and concerns with reduced face-to-face contact. However, these issues could be addressed in initial in-person visits to alleviate concerns and facilitate engagement and motivation in the rehabilitation process. One challenge is that compensatory training is inherently repetitive in nature; thus, measures should be taken to ensure telerehabilitation tools remain accessible and stimulating to avoid disengagement. The authors propose that one approach which may obviate disengagement is to employ feedback and goal setting to improve motivation and provide tangible progress updates.
Patient satisfaction was assessed by Bittner et al31 in a pilot study to develop, administer and evaluate a synchronous virtual low vision portal providing telerehabilitation services. Ten patients diagnosed with either age-related macular degeneration (n=9) or diabetic retinopathy (n=1) were enrolled. Participants were required to have access to a home telephone to use the internet-based video conference portal. Tablet devices were provided as well as MiFi (wireless router which acts as a mobile Wi-Fi hotspot) to enable connection to the internet. Each participant received one telerehabilitation session which lasted approximately 1 hour. The session included administration of the MNREAD chart which consists of a series of 60-character sentences displayed over three lines and is used to assess reading fluency and proficiency using optical magnifiers, using videorecordings and audiorecordings of the participant. Assessments of working distance and lighting were made by the provider viewing the video of the participant reading with their magnifier, whereas assessments of reading speed and accuracy relied on the audio component as participants read aloud during the MNREAD and near acuity tests. The outcomes were participants’ and providers’ audio and video quality ratings. Video quality was rated as excellent to good, whereas audio ratings were more variable. All participants were satisfied and comfortable receiving telerehabilitation and evaluation via videoconferencing. Eight of 10 reported that their magnifier use improved after telerehabilitation. All except one reported that they were very interested in receiving telerehabilitation services again if their visual needs changed.
Lorenzini and Wittich32 reported outcomes related to patient satisfaction in a randomised feasibility study using a head-mounted display and a telehealth platform to deliver synchronous telerehabilitation sessions at home. Participants received real-time distance training sessions delivered by a low vision therapist. The intervention focused on the functional aspects of using eSight eyewear, an assistive technology designed to maximise visual input and compensate for sight loss. The intervention group underwent a personalised training programme including eSkills functional learning activities such as reading, writing and distance vision training. A control group were randomly allocated to conventional eSight self-training using the eSkills user guide. Fifty-seven visually impaired participants were enrolled (experimental group, n=28), the most common causes of sight loss were optic nerve disease, age-related macular degeneration, retinopathy of prematurity and retinitis pigmentosa. Retention rates during the study were 93% (n=53) at 2 weeks, 68% (n=39) at 3 months and 65% (n=37) at 6 months. A higher proportion of patients who withdrew from the study were enrolled into the control group. Participants reported being comfortable with receiving telerehabilitation training at home, with 16 of 23 (66%) agreeing the programme was effective and efficient, and the majority (20 of 23) approving that they would be interested in using telerehabilitation again in the future.
A parallel investigation by Lorenzini and Wittich33 used standardised measures to assess quality of life and patient satisfaction following the eSight telerehabilitation programme. Quality of life outcomes are reported in a later section. Satisfaction was measured using the 12-item Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) tool.41 Scores on the measure increased for participants in both the experimental and control group between baseline and 3 months of device usage, suggesting satisfaction improved independently of the type of training. There were no differences in assistive technology-related satisfaction based on age or sex. Improvement in QUEST scores were not maintained at 6 months. The authors suggest that this may be due to the device no longer meeting certain needs after extended usage, or a lessening impact of social desirability, leading to more realistic and honest responses from participants over time.
Objective visual function
Two studies focused on training related to optimisation of vision delivered through a telerehabilitation service. The studies used visual exploration and ocular movement tasks to activate neuroplasticity to compensate for sight loss. Both studies included patients with measurable visual field loss including areas of diminished sensitivity in glaucoma and hemianopia in stroke patients.
Sabel and Gudlin34 compared outcomes of asynchronous behavioural training using a 1-hour computer-based vision restoration programme for people with glaucoma and a placebo group. Participants were required to have a stable glaucomatous visual field defect inside 30° eccentricity in at least one eye, with well controlled intraocular pressure. After baseline assessments, training was performed 6 days per week for 3 months at home on a commercially available computer with adaptive parameter adjustments. The experimental group performed vision training similar to perimetry whereby visual stimuli of varying luminance are presented in areas of residual vision. The placebo group performed stimulus discrimination training. Vision restoration exercises led to improved vision-related performance in detection accuracy as determined by high-resolution perimetry (p=0.007). Predifferences versus postdifferences after vision training for glaucoma were greater compared with placebo in all perimetry tests (p=0.02 for high-resolution perimetry; p=0.04 for white-on-white perimetry; p=0.04 for blue on yellow perimetry), without affecting eye movements. Moreover, the vision restoration training led to faster reaction time for the glaucoma group (p=0.009). The authors conclude that a telerehabilitation system designed to promote visual system plasticity can be used among older age adults despite widespread visual deterioration, and activation of residual vision may partly reverse vision loss.
A study on patients with hemianopia used a bespoke asynchronous audio–visual telerehabilitation system.35 The system featured a semicircular apparatus in which visual and acoustic stimuli are presented and a central camera to control head and eye movements. Patients used the system at home on a customised tablet which was controlled by a hospital-based therapist. Following an initial assessment in the clinic, participants underwent training at home at least 5 days a week for up to 12 months. The aim of the training was to stimulate multisensory integration mechanisms to reinforce visual and spatial compensatory functions, for example, adoption of oculomotor strategies. Among the sample of three adults with hemianopia, all were capable of actively using the device independently while under remote supervision. Participants showed some improvements in visual detection abilities, which was assessed using two procedures (a unimodal test using only visual stimuli presented at 1 of 12 spatial locations lasting 100 ms and a bimodal audio-visual test whereby visual stimuli was paired with sound), with the strongest effect on both testing procedures observed when participants were free to use eye movements to detect targets, rather than the fixed eye condition.
Quality-of-life, activities of daily living and well-being
Four articles assessed outcomes relating to quality-of-life, activities of daily living, and well-being following telerehabilitation.33 34 36 37 The studies use patient-reported outcome measures and behavioural measurements to examine the benefits of remote interventions in people with vision impairment. Two articles are case reports,36 37 and two articles describe the quality-of-life outcomes from the eSight eyewear,33 and vision restoration training programmes,34 described in an earlier section.
Lorenzini and Wittich33 measure changes in quality-of-life following telerehabilitation with the eSight eyewear programme using the Psychosocial Impact of Assistive Devices Scale (PIADS),42 a 26-item questionnaire composed of three subscales (competence, adaptability and self-esteem) and the Veterans Affairs Low Vision Visual Functioning Questionnaire (VA LV VFQ-48),43 a 48-item instrument used to measure subjective visual outcomes. Visually impaired participants completed the measures at baseline, 2 weeks, 3 months and 6 months. Results patterns were similar across the three subscales of the PIADS showing statistically significantly improved scores after 3 months in both the intervention and control groups (p=0.05), indicating that assistive technology-related quality-of-life (ie, perceived impact of assistive devices on quality-of-life) improved independently of the type of training received. Self-reported functional vision outcomes, as determined by the VA LV VFQ-48, yielded statistically significant improvements in overall scores, as well as in subscales (reading (p=0.03), visual information (p≤0.001), mobility (<0.001)) after 2 weeks of using the device; improvements also continued after 3 months (all p≤0.05).
Sabel and Gudlin’s34 vision restoration programme used the National Eye Institute Visual Function Questionnaire-2544 and the Short-Form-36 (SF-36)45 to measure changes in quality-of-life between baseline and postintervention follow-up. Vision training was not associated with robust changes on these measures. Only the mental health subscale of the SF-36 was found to have improved, which may be caused by non-specific training effects such as attention, alertness or expectation. However, participants had generally scored highly on both measures at baseline, indicating few everyday vision deficits.
A case report by Dogru-Huzmeli et al36 explored whether diplopia complaints could be ameliorated using the Cawthorne-Cooksey exercises applied via telerehabilitation in a multiple sclerosis patient with a visual field scotoma. Cawthorne and Cooksey exercises use a set of eye and head movements which are based on the concept of habituation and designed to build up a tolerance mechanism to support equilibrium and balance.46 47 Exercises were delivered synchronously through WhatsApp video calls over 30 sessions. Comparison of pre eye examinations and post eye examinations suggested gaze restriction, as determined through ophthalmic examination, had improved and that the patient had fewer self-reported double vision complaints. Preintervention and postintervention quality-of-life was assessed using the SF-36 measure of general health. Analysis was based on descriptive reporting of changes in scores, with no statistical analysis reported. The authors report improvement in all domains of the SF-36, except for physical functioning, where there was no change.
A study from Lancioni et al37 assessed whether two congenitally blind women could be supported to make independent phone calls using a computer-aided system. Both women attended a rehabilitation centre where the study took place. The system comprised a netbook computer, which was enabled with a global system for mobile communication with a headset and microphone apparatus. The study adopted an ABAB design in which A represented baseline phases and B represented intervention phases with the telephone system. Communication-related outcomes included the total number of calls made, number of calls met with a response and length of calls. Both participants learnt to use the system and made phone calls independently to a variety of contacts such as family members, friends and care staff personnel, indicating that the intervention may be useful for enabling people with a vision impairment to manage phone calls on their own.
Knowledge relating to ocular symptoms
One study used a telerehabilitation approach to increase knowledge of ocular symptoms to support patients attending a residential school for visually impaired people during the COVID-19 pandemic.38 Senjam et al38 used voice-over internet protocols (eg, WhatsApp calling, Zoom) to enable rehabilitation practitioners at a tertiary eye centre in India to deliver therapeutic education and counselling interventions and monitor ocular complaints among visually impaired adults and children who were unable to attend face-to-face appointments. Over a 2-month study period, 492 patients contacted the team. Health-related complaints were made by 335 patients, the most common ocular complaints being itching (36.1%), watering (16.1%) and painful eyes (3.6%). Counselling sessions addressed uncertainty surrounding clinical monitoring of eye health, however, specific outcomes of counselling were not reported.
Cost-effectiveness
A retrospective cost analysis from Ihrig39 examined the economic practicality of a clinical model of telerehabilitation for visually impaired veterans. Telerehabilitation was delivered by an optometrist and rehabilitation therapist to veterans with conditions including age-related macular degeneration, glaucoma, diabetic retinopathy, cataracts and retinitis pigmentosa. Sessions took place remotely at either the participants’ home or local community outpatient centre. The rehabilitation intervention included home adaptive skills training, which includes a home safety checklist, orientation and mobility training and computer training, as well as training with vision-related activities such as meal management, financial planning, personal care and leisure time activities (Ihrig, 2014).48 Total and median travel cost and time savings were estimated per veteran per fiscal year. Introduction of the telerehabilitation service in 2012 increased access to rural veterans in Western New York. Over a 5-year period, 419 veterans who were unable to access traditional low vision rehabilitation due to travel issues accessed the remote service. The proportion of patients accessing the telerehabilitation service represented 24% of the overall rehabilitation caseload. Median saving of travel miles was 122 miles per veteran (51 136 miles/419 veterans). Median saving of travel time was 2.09 hours per veteran (878 hours/419 veterans). Overall, median travel cost saving per rural individual was US$65.29 per veteran (US$27 357.76/419 veterans). The authors conclude that telerehabilitation can be a practical, time-saving and cost-saving alternative to traditional face-to-face consultations.
Grey literature
Searches of charity websites led to the identification of 11 organisations in the UK where vision rehabilitation services had been shifted to remote delivery during the pandemic. The full list of organisations and the type of services are described in online supplemental material 3. The charities were contacted about their telerehabilitation services and whether any evaluations had been undertaken. This process resulted in the review of seven documents, predominantly internal reports about the restructure of rehabilitation services during the COVID-19 pandemic. While these documents were mostly descriptive, there was useful information demonstrating practice patterns in the third sector. Analysis of grey literature showed that many charities were reviewing their long-term rehabilitation frameworks with an indication that pathways will include a blended approach, offering both remote and face-to-face services on a personalised basis, but require further auditing and evaluation. Most of the organisations described implementing digital skills training to enable beneficiaries to become more proficient with computers and technology, such as making video calls and downloading smartphone applications. There were also examples of internal service evaluations to identify preferences in rehabilitation delivery. For example, Blind Veterans UK, a charity providing support and services to visually impaired UK military veterans, reported information about the needs of their beneficiaries (including emotional support, befriending, assistance with shopping and using technology), methods in delivering remote rehabilitation (including 1:1 interventions such as mindfulness phone sessions and video-based group exercises), and working with allied agencies throughout the COVID-19 pandemic to signpost beneficiaries to support. It was notable that besides a few national sight loss charities (Blind Veterans UK, RNIB), the availability of telerehabilitation appeared to vary greatly, appearing highest within local charities in areas including Cambridgeshire, Leicestershire and Nottinghamshire.
bmjopen-2021-059985supp003.pdf (27.2KB, pdf)
The search of clinical trial databases returned two ongoing trials relevant to telerehabilitation for visually impaired people, which are briefly described here. Van der Aa et al49 (Trial ID: NTR6337) will examine the feasibility of an e-mental health treatment for patients with retinal exudative diseases receiving anti-VEGF treatment. The cognitive behavioural therapy-based intervention is offered via the Internet through the guidance of a social worker. The trial will deliver training and information, which aim to help patients in dealing with their eye condition and managing uncertainties around treatment. The primary outcomes relate to measurements of depression, anxiety and quality-of-life. Another trial (NCT04926974) will evaluate the efficacy of a mobile phone application to improve quality-of-life in older adults with low vision. The application features include real-time remote personal assistance with visual tasks, optical character recognition which allows text to be converted to audio and read aloud, and magnifiers to aid vision. The study seeks to understand the potential of these technologies to improve daily activities, community participation, independence and self-sufficiency in people with low vision. Notably, there are a range of ongoing or completed trials relating to telemonitoring of visually impaired people, such as validation of home-based measurement tools (eg, remote visual field testing). Given such studies are intended to address the broader concept of home monitoring and are not specifically within the context of rehabilitation, these trials were not included.
Trends in publishing
As shown by the results of this review, studies evaluating the impact of telerehabilitation on people with visual impairment are beginning to emerge among the published literature. Yet, these studies represent only a small proportion of the total research on people with vision impairment. For example, a PubMed search for articles with ‘vision impairment’ or ‘blindness’ in the title or abstract yielded 17 783 results since 2010 alone; while in that same period just 10 articles (0.06%) were published that were relevant to telerehabilitation.
Discussion
Vision rehabilitation is a key stage in the eye care journey. Rehabilitative services can help to mitigate the impact of vision loss by equipping patients with new skills and training while providing social connectedness and psychological support.50–54 This review shows that the landscape of rehabilitation is evolving to include synchronous and asynchronous approaches to remote rehabilitation for people with eye conditions. Studies using patient-reported outcome measures suggest telerehabilitation can lead to improved outcomes relating to self-reported daily functioning and quality-of-life.33 34 36 37 In addition, there is generally a high level of acceptability from patients for this shift in service delivery.31–33 However, there remain certain distinct challenges associated with telerehabilitation which may curtail the extent to which this approach is adopted and retained more widely.
Measuring benefits and acceptability of interventions
One difficulty associated with comparing results across studies is the lack of consensus when measuring outcomes. Across all 10 studies identified in this review, 27 different outcome measures were used to assess the benefits of telerehabilitation. These included both performance-based assessments, such as psychometric testing, and subjective or patient-reported measures of health status, visual functioning and quality-of-life. In the four studies which used patient-reported outcomes, just one measure (SF-36) was used in more than one study. An important consideration for clinicians, researchers and trialists could be to aim for a more unified approach when deciding on a core set of outcome measures in future trials and evaluations of telerehabilitation. Second, while it is encouraging that patients’ views and experiences are being considered when measuring the benefits of telerehabilitation, it is important to consider the sensitivity of outcome measures to meaningful changes in areas such as functionality, symptomatology and quality-of-life, etc. For example, the non-significant changes in quality-of-life observed in the study by Sabel and Gudlin34 could be explained by the use of non-disease-specific measures, which may not be sufficiently sensitive to detect small or subtle changes in visual function.55 Finally, the evidence synthesised in this review suggests that telerehabilitation is generally regarded as acceptable by those who are willing to engage with it. Yet, acceptability is a multifaceted concept which may not be fully explained by quantitative behaviour metrics such as the degree of adherence or engagement with an intervention. No studies included in this review describe a framework for acceptability, indicating further research is needed to understand acceptability of telerehabilitation using a robust assessment of relevant factors such as affective attitudes, opportunity costs, ethicality and self-efficacy; thus, future studies investigating acceptability may benefit from a theoretical framework to guide the assessment of acceptability.56
Recommendations and challenges in practice
Several of the studies in this review included recommendations for telerehabilitation which provide helpful insights. For example, a period of direct training with home-based technology was regarded positively, suggesting such training can provide patients with a helpful rehabilitation framework. Despite an increasing number of visually impaired adults engaging with technology,57 it is inevitable that some individuals will have underlying concerns about their technical readiness to operate devices at home. An assessment of individual self-efficacy regarding health management and aptitude for telerehabilitation may, therefore, help to prioritise individuals for whom this approach is most likely to be acceptable and successful.
A key challenge associated with telerehabilitation is maintaining patient motivation and engagement. Rehabilitation is, by nature, highly repetitive and often requires engagement over long periods of time before measurable improvements in areas such as functional vision can be observed. Although studies in this review yielded good patient satisfaction ratings33 and high retention rates,32 it is difficult to predict the sustainability of telerehabilitation outside the context of a research study. For example, devices risk becoming a nuisance if required long term, and while acceptable within research, patients may resist such commitments becoming the standard of care. Similar findings regarding the acceptability of telerehabilitation have been described in a recent systematic review of telerehabilitation for improving adaptive skills in people with multiple disabilities,58 which found that patients are particularly satisfied with the convenience of undergoing rehabilitation from home. However, studies in this review described potentially intensive programmes of telerehabilitation, in some instances requiring several hours of engagement on consecutive days per week. For example, Tinelli et al study’s35 participants were asked to use the telerehabilitation tools for 5 days per week for up to 12 months. Further research using real-world data on patterns of engagement with telerehabilitation will be a valuable addition to the literature and could help to identify factors associated with adherence and withdrawal, and behavioural strategies to encourage adoption.
Cost and capacity considerations
One aspect of telerehabilitation which increases its appeal is the potential for substantial direct and indirect cost savings. The 2019 study by Ihrig39 highlighted that telerehabilitation was associated with considerable time and cost savings for patients by reducing travel requirements and fuel consumption. However, in cases where individual specialist equipment was required, such as the adapted telephone system in the study from Lancioni et al,37 costs per unit were expected to be in the region of US$2000. The economic value of telerehabilitation from a provider perspective requires more research. For example, additional costs may be incurred for services such as training, measurement readings, data management and ongoing maintenance of many devices. Indeed, remote service delivery has been associated with slightly higher costs to service providers, such as speech therapy in people with Parkinson’s disease.59 Nevertheless, it could be expected that remote rehabilitation costs would be largely absorbed by the reduced need for time and resources required for non-remote services. It is noteworthy that telerehabilitation may have a wider reach than standard rehabilitation services, and the increased availability and convenience of a remote service may be more appealing to a broader profile of patients (eg, working age individuals with minimal time for in-person sessions). As shown by Ihrig,39 remote service delivery led to an average workload increase of 24% due to a higher number of patients accessing the service. If this finding applied to a broader audience, there will likely be a larger rehabilitation patient caseload, with possible capacity implications for clinical practice.
Limitations of identified studies
Although no studies were formally excluded on the basis of insufficient quality (inclusion threshold set at 55% (0.55)), some common study limitations were identified. The most frequent issues with the studies according to the Kmet et al checklist was the presence of only a partial description of subject characteristics (2 of 10) and study conclusions not being fully supported by the data (3 of 10). Additionally, the majority of the studies introduce a self-selection bias when participants elect to take part in research and are willing to engage with telerehabilitation programmes. Although common in cross-sectional research, self-selection bias can complicate the interpretation of study data as participants’ propensity for participating in research may correlate with the topic under investigation. For example, Lorenzini and Wittich32 report that 79% of eligible participants declined to take part in the study. As such, the conclusions are based on a relatively small proportion of the target population. Reasons for non-participation were seldom discussed in the published reports; therefore, it is unclear whether factors such as level of familiarity with devices, visual functioning, extent of sight impairment or having assistance from a sighted friend or family member impact on engagement with telerehabilitation. In addition, the studies in this review report the outcomes of telerehabilitation after a relatively short period of time (ie, less than 1 year). As observed by Lorenzini and Wittich,32 engagement is more likely to decrease after 6 months, highlighting the need for more longitudinal studies. A further common limitation was the relatively small sample sizes observed in the studies. For example, 4 of the 10 studies included in this review had a sample size of 10 or fewer. Although this review set out to describe the type of telerehabilitation for people with vision impairment, participants across the identified studies were mostly low vision patients with mild or moderate visual loss; therefore, the findings may not extend to other subgroups within the vision impairment population, such as those with severe sight impairment or no perception of light. There are currently very few randomised controlled clinical trials evaluating patient outcomes in telerehabilitation, for example, 3 of the 10 studies identified in this review used random allocation to an intervention and control group,32–34 and we propose this would be an important avenue for further research, as well as comparisons between traditional face-to-face and telerehabilitation services to understand the challenges associated with telerehabilitation in the specific context of visual impairment.
Limitations
This review’s methodology has a number of limitations. Only articles written in English were screened and ultimately included, thus excluding potentially relevant studies in languages other than English. However, only three studies were excluded for this reason. Moreover, included studies were required to relate to some form of visual impairment, and several studies included heterogeneous samples of varying or unknown degrees of sight loss from numerous conditions. A range of vision impairment terms were used across the studies including ‘sight loss’, ‘blindness’ and ‘low vision’. Results were rarely disaggregated by disease severity or type, thereby making it difficult to account for potential nuances between different patient groups under the broad overarching term of ‘vision impairment’. A key strength of this review was the inclusion of grey literature. Grey literature includes a range of documents not controlled by commercial publishing organisations and can be a rich source of information which cannot be obtained from other sources.60 This review highlights that the availability of telerehabilitation through local charity networks appeared to vary depending on location. While a paucity of online documentation regarding charity telerehabilitation services in some regions does not necessarily equate to an absence of such services, it does suggest a possible unevenness in their availability across local authorities. This may reflect broader issues pertaining to unequal access to sight loss support nationwide. As telerehabilitation continues to emerge as an effective and potentially permanent fixture in the care pathways of visually impaired people, there is a need to bridge the gaps in service delivery to ensure there is equitable provision across all areas of the UK, particularly given the potential for a wider geographical reach with remote services thereby increasing access to support.
Conclusions
In summary, the COVID-19 pandemic necessitated a redesign of traditional face-to-face rehabilitation pathways to remote service delivery. A previous systematic review assessing the effectiveness of low vision telerehabilitation found no studies had been completed in this area.23 We identified a range of remote-based rehabilitation services aimed at optimising vision and encouraging adjustment to sight loss, with evidence to suggest some patients are generally accepting of this model and may benefit from improved functional and quality-of-life outcomes, while potentially offering a more cost-effective approach to continuing care. The weight of the evidence suggests telerehabilitation has a promising role in patient care pathways for people with a visual impairment; however, issues around long-term desirability and compliance remain unclear. Given the variability in patients’ aptitude and motivation to sustainably engage with telerehabilitation, a self-select approach which allows patients to choose their preferred mode of rehabilitation delivery or individualised interventions may be the most practical means of ensuring effective implementation of remote services. This review has addressed increasingly relevant questions about the role of telerehabilitation when applied among people with vision impairment. The findings to date illustrate the benefits of remote rehabilitation services, but more research is needed to better understand its overall effectiveness, scalability and longevity. Ultimately, we hope this review can inform key stakeholders, including hospital eye services, community groups and charities about priority areas for future research and development.
Supplementary Material
Footnotes
Twitter: @jones_lee1, @renatasmgomes
Contributors: All authors made substantial contributions to the design and analysis of the work. LJ and ML performed the literature search, article screening, data extraction, quality appraisal and manuscript preparation. CLC, NH and RSMG conceptualised the review and edited the manuscript. All authors approved the final manuscript. RSMG is the guarantor.
Funding: This work was supported by the Thomas Pocklington Trust, grant number TP-211.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval for this scoping review was not required.
References
- 1.Pezzullo L, Streatfeild J, Simkiss P, et al. The economic impact of sight loss and blindness in the UK adult population. BMC Health Serv Res 2018;18:63. 10.1186/s12913-018-2836-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Royal National Institute of Blind People (RNIB) . The criteria for registration. Available: www.rnib.org.uk/eye-health/registering-your-sight-loss/criteria-certification [Accessed 6 Dec 2021].
- 3.Chiang PPC, Zheng Y, Wong TY, et al. Vision impairment and major causes of vision loss impacts on vision-specific functioning independent of socioeconomic factors. Ophthalmology 2013;120:415–22. 10.1016/j.ophtha.2012.07.077 [DOI] [PubMed] [Google Scholar]
- 4.Taylor DJ, Hobby AE, Binns AM, et al. How does age-related macular degeneration affect real-world visual ability and quality of life? A systematic review. BMJ Open 2016;6:e011504. 10.1136/bmjopen-2016-011504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fenwick EK, Ong PG, Man REK, et al. Association of vision impairment and major eye diseases with mobility and independence in a Chinese population. JAMA Ophthalmol 2016;134:1087–93. 10.1001/jamaophthalmol.2016.2394 [DOI] [PubMed] [Google Scholar]
- 6.Swenor BK, Simonsick EM, Ferrucci L. And health, aging and body composition study. visual impairment and incident mobility limitations: the health, aging and body composition study. J Am Geriatr Soc 2015;63:46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones L, Bryan SR, Crabb DP. Gradually then suddenly? Decline in vision-related quality of life as glaucoma worsens. J Ophthalmol 2017;2017:1621640. 10.1155/2017/1621640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langelaan M, de Boer MR, van Nispen RMA, et al. Impact of visual impairment on quality of life: a comparison with quality of life in the general population and with other chronic conditions. Ophthalmic Epidemiol 2007;14:119–26. 10.1080/09286580601139212 [DOI] [PubMed] [Google Scholar]
- 9.Burton AE, Gibson JM, Shaw RL. How do older people with sight loss manage their general health? A qualitative study. Disabil Rehabil 2016;38:2277–85. 10.3109/09638288.2015.1123310 [DOI] [PubMed] [Google Scholar]
- 10.Hinds A, Sinclair A, Park J, et al. Impact of an interdisciplinary low vision service on the quality of life of low vision patients. Br J Ophthalmol 2003;87:1391–6. 10.1136/bjo.87.11.1391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organisation . Rehabilitation. Available: who.int [Accessed 5 May 2022].
- 12.Latham K, Macnaughton J. Low vision rehabilitation needs of visually impaired people. Optomet Pract 2017;18:103–10. [Google Scholar]
- 13.American Academy of Ophthalmology Vision Rehabilitation Committee . Preferred practice pattern guidelines. vision rehabilitation for adults. San Francisco, CA: American Academy of Ophthalmology, 2013. www.aao.org/ppp [Google Scholar]
- 14.van Nispen RM, Virgili G, Hoeben M, et al. Low vision rehabilitation for better quality of life in visually impaired adults. Cochrane Database Syst Rev 2020;1:CD006543. 10.1002/14651858.CD006543.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rees G, Ponczek E, Hassell J, et al. Psychological outcomes following interventions for people with low vision: a systematic review. Expert Rev Ophthalmol 2010;5:385–403. 10.1586/eop.10.32 [DOI] [Google Scholar]
- 16.Chung STL. Enhancing visual performance for people with central vision loss. Optom Vis Sci 2010;87:276–84. 10.1097/OPX.0b013e3181c91347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brennan D, Tindall L, Theodoros D, et al. A blueprint for telerehabilitation guidelines. Int J Telerehabil 2010;2:31–4. 10.5195/ijt.2010.6063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mechanic OJ, Persaud Y, Kimball AB. Telehealth systems. In: StatPearls. Treasure Island, FL: StatPearls Publishing, 2020. www.ncbi.nlm.nih.gov/books/NBK459384/ [PubMed] [Google Scholar]
- 19.McCue M, Fairman A, Pramuka M. Enhancing quality of life through telerehabilitation. Phys Med Rehabil Clin N Am 2010;21:195–205. 10.1016/j.pmr.2009.07.005 [DOI] [PubMed] [Google Scholar]
- 20.Cottrell MA, Galea OA, O'Leary SP, et al. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil 2017;31:625–38. 10.1177/0269215516645148 [DOI] [PubMed] [Google Scholar]
- 21.Yeroushalmi S, Maloni H, Costello K, et al. Telemedicine and multiple sclerosis: a comprehensive literature review. J Telemed Telecare 2020;26:400–13. 10.1177/1357633X19840097 [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, Abel KT, Janecek JT, et al. Home-based technologies for stroke rehabilitation: a systematic review. Int J Med Inform 2019;123:11–22. 10.1016/j.ijmedinf.2018.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bittner AK, Yoshinaga PD, Wykstra SL, et al. Telerehabilitation for people with low vision. Cochrane Database Syst Rev 2020;2:CD011019. 10.1002/14651858.CD011019.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc 2020;27:957–62. 10.1093/jamia/ocaa067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic - United States, January-March 2020. MMWR Morb Mortal Wkly Rep 2020;69:1595–9. 10.15585/mmwr.mm6943a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 27.Higgins JP, Thomas J, Chandler J, eds. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, 2019. [Google Scholar]
- 28.Baumann N. How to use the medical subject headings (MeSH). Int J Clin Pract 2016;70:171–4. 10.1111/ijcp.12767 [DOI] [PubMed] [Google Scholar]
- 29.Kmet LM, Lee RC, Cook LS. HTA Initiative #13. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. HTA Initiative, 2004. Available: https://www.ihe.ca/advanced-search/standard-quality-assessment-criteria-for-evaluating-primary-research-papers-from-a-variety-of-fields
- 30.Dunne S, Close H, Richards N, et al. Maximizing telerehabilitation for patients with visual loss after stroke: interview and focus group study with stroke survivors, carers, and occupational therapists. J Med Internet Res 2020;22:e19604. 10.2196/19604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bittner AK, Yoshinaga P, Bowers A, et al. Feasibility of telerehabilitation for low vision: satisfaction ratings by providers and patients. Optom Vis Sci 2018;95:865–72. 10.1097/OPX.0000000000001260 [DOI] [PubMed] [Google Scholar]
- 32.Lorenzini M-C, Wittich W. Personalized telerehabilitation for a head-mounted low vision aid: a randomized feasibility study. Optom Vis Sci 2021;98:570–81. 10.1097/OPX.0000000000001704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorenzini M-C, Wittich W. Head-Mounted visual assistive technology-related quality of life changes after telerehabilitation. Optom Vis Sci 2021;98:582–91. 10.1097/OPX.0000000000001705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabel BA, Gudlin J. Vision restoration training for glaucoma: a randomized clinical trial. JAMA Ophthalmol 2014;132:381–9. 10.1001/jamaophthalmol.2013.7963 [DOI] [PubMed] [Google Scholar]
- 35.Tinelli F, Cioni G, Purpura G. Development and implementation of a new telerehabilitation system for audiovisual stimulation training in hemianopia. Front Neurol 2017;8:621. 10.3389/fneur.2017.00621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dogru-Huzmeli E, Duman T, Cakmak AI, et al. Can diplopia complaint be reduced by telerehabilitation in multiple sclerosis patient during the pandemic?: a case report. Neurol Sci 2021;42:1–4. 10.1007/s10072-021-05194-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lancioni GE, O'Reilly MF, Singh NN, et al. Enabling two women with blindness and additional disabilities to make phone calls independently via a computer-aided telephone system. Dev Neurorehabil 2011;14:283–9. 10.3109/17518423.2011.586372 [DOI] [PubMed] [Google Scholar]
- 38.Senjam SS, Manna S, Vashist P, et al. Tele-rehabilitation for visually challenged students during COVID-19 pandemic: lesson learned. Indian J Ophthalmol 2021;69:722. 10.4103/ijo.IJO_2527_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ihrig C. Travel cost savings and practicality for low-vision telerehabilitation. Telemed J E Health 2019;25:649–54. 10.1089/tmj.2018.0092 [DOI] [PubMed] [Google Scholar]
- 40.Aimola L, Lane AR, Smith DT, et al. Efficacy and feasibility of home-based training for individuals with homonymous visual field defects. Neurorehabil Neural Repair 2014;28:207–18. 10.1177/1545968313503219 [DOI] [PubMed] [Google Scholar]
- 41.Demers L, Weiss-Lambrou R, Ska B. Development of the Quebec user evaluation of satisfaction with assistive technology (QUEST). Assist Technol 1996;8:3–13. 10.1080/10400435.1996.10132268 [DOI] [PubMed] [Google Scholar]
- 42.Day H. Measuring the psychosocial impact of assistive devices: the PIADS. Canadian J Rehabilit 1996;9:159–68. [Google Scholar]
- 43.Stelmack JA, Szlyk JP, Stelmack TR, et al. Psychometric properties of the Veterans Affairs low-vision visual functioning questionnaire. Invest Ophthalmol Vis Sci 2004;45:3919–28. 10.1167/iovs.04-0208 [DOI] [PubMed] [Google Scholar]
- 44.Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol 2001;119:1050–8. 10.1001/archopht.119.7.1050 [DOI] [PubMed] [Google Scholar]
- 45.Ware JE. SF-36 health survey update. Spine 2000;25:3130–9. 10.1097/00007632-200012150-00008 [DOI] [PubMed] [Google Scholar]
- 46.Cawthorne T. Vestibular injuries. Proc R Soc Med 1946;39:270–3. 10.1177/003591574603900522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cooksey FS. Rehabilitation in vestibular injuries. Proc R Soc Med 1946;39:273–8. 10.1177/003591574603900523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ihrig C. Rural healthcare pilot clinic: low vision clinical video telehealth. J Assoc Schools Colleges Optomet 2014;40:14–16. [Google Scholar]
- 49.van der Aa HPA, van Rens GHMB, Verbraak FD, et al. Economic evaluation of an e-mental health intervention for patients with retinal exudative diseases who receive intraocular anti-VEGF injections (E-PsEYE): protocol for a randomised controlled trial. BMJ Open 2017;7:e018149. 10.1136/bmjopen-2017-018149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haymes SA, Johnston AW, Heyes AD. Preliminary investigation of the responsiveness of the Melbourne low vision ADL index to low-vision rehabilitation. Optom Vis Sci 2001;78:373–80. 10.1097/00006324-200106000-00008 [DOI] [PubMed] [Google Scholar]
- 51.Reeves BC, Harper RA, Russell WB. Enhanced low vision rehabilitation for people with age related macular degeneration: a randomised controlled trial. Br J Ophthalmol 2004;88:1443–9. 10.1136/bjo.2003.037457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Horowitz A, Reinhardt JP, Boerner K. The effect of rehabilitation on depression among visually disabled older adults. Aging Ment Health 2005;9:563–70. 10.1080/13607860500193500 [DOI] [PubMed] [Google Scholar]
- 53.Stelmack JA, Szlyk JP, Stelmack TR, et al. Measuring outcomes of vision rehabilitation with the veterans affairs low vision visual functioning questionnaire. Invest Ophthalmol Vis Sci 2006;47:3253–61. 10.1167/iovs.05-1319 [DOI] [PubMed] [Google Scholar]
- 54.Binns AM, Bunce C, Dickinson C, et al. How effective is low vision service provision? A systematic review. Surv Ophthalmol 2012;57:34–65. 10.1016/j.survophthal.2011.06.006 [DOI] [PubMed] [Google Scholar]
- 55.Jones L, Garway-Heath DF, Azuara-Blanco A, et al. Are patient self-reported outcome measures sensitive enough to be used as end points in clinical trials?: evidence from the United Kingdom Glaucoma Treatment Study. Ophthalmology 2019;126:682–9. 10.1016/j.ophtha.2018.09.034 [DOI] [PubMed] [Google Scholar]
- 56.Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Servic Res 2017;17:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ali ZC, Shakir S, Aslam TM. Perceptions and use of technology in older people with ophthalmic conditions. F1000Res 2019;8:86. 10.12688/f1000research.17181.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Caprì T, Nucita A, Iannizzotto G, et al. Telerehabilitation for improving adaptive skills of children and young adults with multiple disabilities: a systematic review. Rev J Autism Dev Disord 2021;8:244–52. 10.1007/s40489-020-00214-x [DOI] [Google Scholar]
- 59.Saiyed M, Hill AJ, Russell TG. Cost analysis of home telerehabilitation for speech treatment in people with Parkinson’s disease. J Telemed Telecare 2020;26:1–6. [DOI] [PubMed] [Google Scholar]
- 60.Adams J, Hillier-Brown FC, Moore HJ, et al. Searching and synthesising ‘grey literature’ and ‘grey information’ in public health: critical reflections on three case studies. Syst Rev 2016;5:164. 10.1186/s13643-016-0337-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059985supp001.pdf (63.3KB, pdf)
bmjopen-2021-059985supp002.pdf (74.8KB, pdf)
bmjopen-2021-059985supp003.pdf (27.2KB, pdf)
Data Availability Statement
No data are available.