Abstract
Introduction
Postoperative pain remains a challenging medical condition impacting the quality of life of every patient. Although several predictive factors for postoperative pain have been identified, an adequate prediction of postoperative pain in patients at risk has not been achieved yet.
The primary objective of this study is to identify specific genetic risk factors for the development of acute and chronic postoperative pain to construct a prediction model facilitating a more personalised postoperative pain management for each individual. The secondary objectives are to build a databank enabling researchers to identify other risk factors for postoperative pain, for instance, demographic and clinical outcome indicators; provide insight into (genetic) factors that predict pharmacological pain relief; investigate the relationship between acute and chronic postoperative pain.
Methods and analysis
In this prospective, observational study, patients who undergo elective surgery will be recruited to a sample size of approximately 10 000 patients. Postoperative acute and chronic pain outcomes will be collected through questionnaires at different time points after surgery in the follow-up of 6 months. Potential genetic, demographic and clinical risk factors for prediction model construction will be collected through blood, questionnaires and electronic health records, respectively.
Genetic factors associated with acute and/or chronic postoperative pain will be identified using a genome-wide association analysis. Clinical risk factors as stated in the secondary objectives will be assessed by multivariable regression. A clinical easy-to-use prediction model will be created for postoperative pain to allow clinical use for the stratification of patients.
Ethics and dissemination
The Institutional Review Board of the Radboud university medical centre approved the study (authorisation number: 2012/117). The results of this study will be made available through peer-reviewed scientific journals and presentations at relevant conferences, which will finally contribute to personalised postoperative pain management.
Trial registration number
Keywords: PAIN MANAGEMENT, GENETICS, SURGERY, EPIDEMIOLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This is a large prospective study to identify genetic and other risk factors for postoperative pain.
We will build a databank with comprehensive interdisciplinary measurements that assess postoperative pain from multiple perspectives.
Outcome measurements of pain by patient-reported outcomes, rather than evaluated by professionals.
The investigating biomarkers of postoperative pain are limited to genetic variants.
Introduction
Pain after surgery remains a challenging medical and societal problem.1 Pain is one of the most common postsurgical side effects, with moderate to severe acute postoperative pain occurring in about 41% of the patients.2–4 Severe postoperative pain is associated with an increased incidence of postoperative complications,5 including prolonged hospital stay, readmissions and significant reduction of patient satisfaction and quality of life.6 7 In addition, acute postoperative pain is associated with chronic pain development after surgery.8 A recent position paper from the International Association for the Study of Pain (IASP) stated that among the almost 40 million people undergoing surgery globally each year, 1 out of 10 develops chronic postsurgical pain (CPSP), and 1 out of 100 suffers from severe CPSP, which will negatively affect patients’ quality of life.9 In addition, postoperative pain is a considerable burden on healthcare service costs, both directly due to patients’ increased consumption of medical care and indirectly due to absenteeism, reduced productivity and increased social welfare payments.10–15
The management of both acute postoperative pain2 16 and CPSP2 17 has remained suboptimal. Despite major investments in clinical protocols and guidelines for structural pain management, infrastructure and acute pain services, no significant outcome improvements in the quality of postoperative pain management for individual patients have been achieved in the last 15 years.10 11
Given the high incidence of postoperative pain, identifying patients at risk for CPSP before the operation is important to apply more personalised pain prevention strategies. The most important demographic and clinical risk factors for postoperative pain are younger age, female sex, smoking, history of depressive symptoms, anxiety symptoms, sleep difficulties, higher body mass index (BMI), presence of preoperative pain and use of preoperative analgesics.18 Based on these factors, models have been developed to predict severe acute postoperative pain19 20 and CPSP.21 22 A recent study has evaluated a presurgical risk score for CPSP in a prospective cohort, and it reliably identified about 70% of the patients undergoing surgeries at risk of CPSP.23 24
As a multifactorial trait, the incidence variation of CPSP in the population can be explained partly by the demographic and clinical risk factors mentioned above, and partly due to the genetic and epigenetic differences among patients.25 26 To improve the accuracy and power of prediction, efforts have been made to predict CPSP using genetic variants.21 24 However, no unequivocal genetic predictors have been found yet. In addition, many exploratory studies investigated the possible role of candidate genes in postoperative pain development. In particular, associations have been found between CPSP and the µ-opioid receptor (OPRM1) and catechol-O-methyl transferase (COMT) genes.27 28 Still, these results have not been confirmed by others. OPRM1 is also associated with basal pain sensitivity differences,29 which could be caused by the altered opioid binding potential in the central nervous system.30 More recently, hypothesis-free methods, such as Genome-Wide Association (GWA) studies (GWAS), have been applied for CPSP to identify markers across the genome.31 32 One of the studies showed that a genetic variant in the protein-kinase C gene is linked to neuropathic pain after complete joint replacement. This gene is involved in long-term potentiation, synaptic plasticity, chronic pain and memory, indicating that this gene may be relevant for neuropathic pain initiation. The disadvantage of this study is that it was small in terms of patient numbers and only focused on one specific surgical procedure.
Besides genetic variants for altered pain sensitivity, gene variants in drug metabolism can also play a role. Understanding the reasons for ineffective treatment can facilitate the early identification of patients at risk and provide more effective and customised postoperative management. Some associated genes with pain treatment outcomes are also involved in pain development, such as COMT.33–35 Genes involved in the action site of active drugs or the drugs’ metabolism might play a role in the therapeutic response of this drug. A well-known example is the cytochrome P450 (CYP) family investigated for several drugs (eg, codeine and tramadol).36 However, this area has never been charted in a large population.37
To date, adequate prediction of patients at risk for postoperative pain in clinical practice has not been achieved for several reasons. First, although many demographic, clinical and lifestyle factors of postoperative pain have been reported,18 a lack of consensus on the best outcome indicators for postoperative pain management38 39 hinders choosing the proper outcome variables for prediction model construction. Second, the potential genetic risk factors of postoperative pain prediction remain obscure. The role of genetic factors in postoperative pain have not been investigated sufficiently, making it challenging to select appropriate genetic risk factors to construct a prediction model. Third, when prediction models are updated, external validation (ie, in a new population) is important before being implemented in a clinical setting,40–43 which is often difficult due to the lack of validation cohorts. For these reasons, we hypothesise that a global structural multicentre diagnostic programme of postoperative pain in a surgical patient population will be valuable for better identifying patients at risk of CPSP and ultimately preventing postoperative pain using individualised pharmacological and non-pharmacological interventions.
Objectives
The primary objective of the Pain Predict Genetics (PPG) study is to identify genetic risk factors for acute and chronic postoperative pain development and to construct a prediction model for personalised postoperative pain management.
The secondary objectives of the PPG study are to build a databank enabling researchers to (1) identify other risk factors for the development of acute and chronic postoperative pain; (2) provide insights into complications and other clinical outcome indicators after surgery; (3) provide insights into the relationship between acute and chronic postoperative pain and (4) identify (genetic) factors that predict pharmacological pain relief. The databank will be open to the public with access fees, and reasonable requests will be discussed in the research group before approval.
The extensive data collection on (chronic) postoperative pain development of patients undergoing surgery offers many possibilities for additional research questions using conventional statistical methods and artificial intelligence, for example, machine learning. The cohort could be used to (1) conduct epidemiological studies; (2) investigate other parameters (eg, types of surgery) that are involved in the development of chronic postoperative pain; (3) validate new prediction models for (chronic) postoperative pain; (4) identify factors for the postoperative outcome (for example, death, long-term hospitalisation, complications); (5) collaborate with other groups to perform large-scale analysis to identify predictors for the development of (chronic) postoperative pain.
Methods and analyses
Study design
A prospective, observational study of 10 000 patients will undergo elective surgery. This study will run for at least ten years, during which period it must be possible to include the intended number of patients. Patient inclusion after CMO (Human Research Committee, in Dutch Commissie Mensgebonden Onderzoek) approval was started in March 2015, and patient inclusion was temporarily stopped in 2020 due to COVID-19 restrictions. In the near future, this study will be continued as a multicentre study; hospitals have already been approached and indicated that they intend to participate.
Patient and public involvement
During the design of the study, the patients aided in the pilot phase of the questionnaires; during the recruitment the patients are informed concerning the project. In addition, patient reported outcomes will be used. Patients will be informed about the outcome of the study at several moments (depending on the obtained results).
Participants
Patients who undergo electvie surgry and are eligible for this study will be approached before their planned surgery during the preoperative consultation. In this way, potential participants will have sufficient time to consider the study information. If any questions arise, it is possible to contact the researchers by telephone or ask the questions during the preoperative consultation. During the preoperative consultation (outpatient clinic or by telephone), the physician (assistant) will ask the patient if they are interested to participating in the study. If the patient is willing to participate, the informed consent form will be signed and dated. If patients have an online preoperative consultation, this procedure will take place digitally, and patients receive the study forms (signed in advance) at home to return if they consent.
Patients are eligible for study inclusion if they (1) are older or equal to 16 years; (2) undergo elective surgery with an incision, including cardiothoracic surgery (eg, cardiomyotomy), general surgery (eg, breast resection), neurological surgery (eg, nerve decompression), oral and maxillofacial surgery (eg, removal of head and neck benign and malignant tumours), otorhinolaryngology (eg, tympanoplasty), plastic surgery (eg, breast reconstruction), trauma and orthopaedic surgery (eg, arthroplasty), urology (eg, prostatectomy) and vascular surgery (eg, treatment of varicose veins); (3) can read and understand the patient information; (4) will provide informed consent. Patients will be excluded if they (1) intend to undergo another surgery within 6 months and (2) do not have enough knowledge of the language in words and understanding to complete questionnaires.
Measurements
Questionnaires
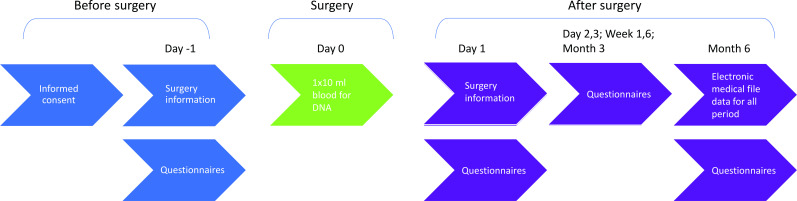
After written informed consent, participants will be asked to complete questionnaires before and after their surgery. An overview of the study workflow and data collection time points can be found in figure 1 and table 1. All patient data will be stored in an online digital database, Castor.44 The reliability and validity of all questionnaires for measurement collection have been validated in the corresponding populations.
Figure 1.
Pain predict genetics study design overview. After written informed consent, participants will be asked to complete questionnaires before and after their surgery. One tube of blood will be collected for DNA isolation using the intravenous line in place for surgery. Clinical information will be collected from the electronic patient file after the operation.
Table 1.
Overview of data collection
| T0 | Day −1 | Surgery | Day 1 | Day 2 | Day 3 | Week 1 | Week 6 | Month 3 | Month 6 | |
| Informed consent | x | |||||||||
| Questionnaires | ||||||||||
| Demografic data | x | |||||||||
| Incision size | x | x | ||||||||
| Pain scores | x | x | x | x | x | x | x | x | ||
| Physical activities | x | x | x | x | ||||||
| Pain Disability Index | x | x | x | x | x | |||||
| APAIS | x | |||||||||
| PCS | x | |||||||||
| PSQ | x | |||||||||
| Chronic pain | x | x | x | |||||||
| IDS depression | x | |||||||||
| Brief pain inventory | x | x | ||||||||
| Data electronic medical file | ||||||||||
| Physical status by ASA | x | |||||||||
| Type of surgery | x | |||||||||
| Duration of surgery | x | |||||||||
| Type of anaesthesia | x | |||||||||
| Complications | x | |||||||||
| Hospital stay | x | |||||||||
| Pain medication use | x | |||||||||
| Incision size | x | |||||||||
| Second surgery within 6 months | x | |||||||||
| General clinical outcome indicators | x | |||||||||
| Body material* | ||||||||||
| 1×10 mL blood for DNA | x | |||||||||
*In the event that it is not possible to collect a blood sample during surgery, the subject may be asked to provide a DNA sample via a saliva collection tube.
APAIS, Amsterdam Pre-operative Anxiety and Information Scale; ASA, American Society of Anesthesiologists classification; IDS, Inventory of Depressive Symptomatology; PCS, Pain Catastrophising Scale; PSQ, Pain Sensitivity Questionnaire.
The first digital questionnaire must be completed the day before the surgery (no longer than 1 week before). Before surgery, the following parameters will be collected (table 1, online supplemental file 1): demographic characteristics (such as gender, age, BMI), expected incision size in mm, pain intensity, pain disability, preoperative anxiety and need for information, pain catastrophising, pain sensitivity, preoperative chronic pain characteristics and depressive symptoms.
bmjopen-2022-066134supp001.pdf (404.8KB, pdf)
After surgery, the following parameters will be collected: actual incision size in mm on day 1; pain intensity on days 1, 2, 3, weeks 1 and 6, and months 3 and 6; physical activities on days 1, 2, 3, week 1; pain disability on weeks 1 and 6, and months 3 and 6; postoperative chronic pain characteristics on months 3 and 6; characteristics of pain on months 3 and 6.
Pain intensity will be measured with an 11-point Numerical Rating Scale (NRS) at rest and during a normal patient action at that time.20 The endpoints represent the extremes of the pain experience: 0 means ‘no pain at all’ and 10 means ‘worst possible pain’.
Pain disability (disability associated with pain) will be measured by the widely used Pain Disability Index Dutch language version (PDI).45 46 The PDI is a seven-item questionnaire to investigate the magnitude of the self-reported disability in different situations such as work, leisure time, daily life activities and sports. The questionnaire is constructed on an 11-point NRS in which 0 means ‘no disability’ and 10 means ‘maximum disability’.
Preoperative anxiety and need for information will be evaluated by the Amsterdam Preoperative Anxiety and Information Scale (APAIS).47 The APAIS consists of six questions and each score on a five-point Likert scale from 1 (not at all) to 5 (extremely), with four questions to assess the patient’s preoperative anxiety score and two questions to assess the patient’s need for information regarding the scheduled surgery and anaesthesia.20
Pain catastrophising is generally described as an absurd negative orientation towards hurtful stimuli and is important in pain coping.48 It will be measured by the Pain Catastrophising Scale, a self-evaluating questionnaire consisting of 13 questions. People are asked to indicate the degree to which they have thoughts and feelings when experiencing pain using the 0 (not at all) to 4 (all the time) scale, and a total score will be yielded (range from 0 to 52).
The Pain Sensitivity Questionnaire (PSQ) will measure patients’ preoperative pain sensitivity.49 50 The PSQ consists of 17 questions that describe daily life situations; respondents score their pain intensity for these situations on an NRS by scoring 0 (not painful) to 10 (severest pain imaginable).
The severity of overall depressive symptoms will be assessed by the Inventory of Depressive Symptomatology Self Report (IDS-SR).51 52 IDS-SR is a 30-item questionnaire, and each item has four statements scored on a four-point scale from 0 to 3. There are two items about either increasing or decreasing appetite and two items about increasing or decreasing weight. Only the item with the higher score from both pairs will be chosen. The total score is based on 28 items and ranges from 0 to 84.
Physical activities (ability to perform normal activities) will be measured by questions assessing the degree of physical activities interfered by surgery, including bed activities (such as turning), breathing deeply of coughing, sleeping and activities out of bed. Each item is scored on an 11-point NRS in which 0 means did not interfere and 10 means completely interfered. These questions are derived from the validated International Pain Outcomes questionnaire and are found responsive to asking patients about their ability to perform normal activities directly after surgery.53
Characteristics of pain will be measured by the Brief Pain Inventory-Short Form (BPI-SF), which is a shortened version of the BPI.54 BPI-SF evaluates pain severity during the past 24 hours and current level, with 0 representing ‘no pain’ and 10 ‘the worst pain imaginable’. Seven items in BPI-SF assess interference with daily functioning (such as general activity, walking and work) on an 11-point scale, where 0 represents ‘no interference’ and 10 ‘complete interference’.
Collection of body material
One tube of blood will be collected for DNA isolation. The burden for the patient is minimalised as blood will be taken using the intravenous line in place for surgery. If it is impossible to collect blood presurgically or postsurgically, we will collect saliva for DNA isolation (Genefix DNA saliva collectors; GFX-02/50, Isohelix).
Clinical information
The following clinical information will be collected from the electronic patient file six months after operation (table 1): physical status by The American Society of Anesthesiologists classification status; type of surgery; duration of surgery; type of anaesthesia; postoperative complications within 30 days after surgery, one-time retrospectively, which is defined as any medical adverse outcome occurring between admission and 30 days after operation. Complications occurring in the operation room and complications directly related to anaesthesia (eg, nausea which resolves immediately after medication in the operation room) will not be included.5 55 Furthermore, data on pain medication use, before surgery and after surgery; actual incision size in mm; second surgery within 6 months; general clinical outcome indicators, including surgical site infection at 30 days, stroke within 30 days of surgery, death within 30 days of surgery, admission to the intensive care unit within 14 days of surgery, readmission to hospital within 30 days of surgery and length of hospital stay (with or without in-hospital mortality) will be collected.38
Outcome measures
The outcome measures are acute postoperative pain and chronic postoperative pain. Acute postoperative pain is defined as pain experienced directly after surgery. Thresholds or cut-off points of the pain intensity are set as none to mild (0–3), moderate (4–7) and severe (8–10).56 57 The definition of CPSP is in agreement with IASP terminology of CPSP, that is, ‘chronic pain that develops or increases in intensity after a surgical procedure persists beyond the healing process, that is, at least 3 months after the surgery’.9 CPSP will be measured by a chronic pain characteristics questionnaire postoperatively at 3 and 6 months. Patients will be asked to indicate whether they had a recent pain experience, the site of pain and whether it lasted more than 3 months.58 59 The intensity of CPSP will also be characterised by the pain scores questionnaire using the same threshold as acute postoperative pain. The influence of pain on functional and mood changes will be measured by the PDI and the BPI-SF.
Sample size calculation
The power of the genetic study is based on the primary research question investigating which genetic factors are associated with postoperative pain. Power is calculated using the Genetic Power Calculator,60 and the estimated number of patients is based on a GWA approach. For chronic postoperative pain, we assume a case–control analysis for discrete traits (2 df test), a risk allele frequency of 30%, a linkage disequilibrium (D') of 0.8, a prevalence of chronic postoperative pain of 15%, and the relative risk of chronic postoperative pain for persons who are heterozygous of 1.5 and for homozygous persons of 2.25. For a power of 80% with a p value cut-off 5×10−8 (genome-wide significance threshold), we need 750 patients with chronic postoperative pain and 4250 people without chronic postoperative pain. For acute pain, the power is even higher. With the same population, we have more than 80% power to detect a relative risk of 1.2 and 1.44 for heterozygous and homozygous patients, respectively. This higher power is due to the higher prevalence of acute (moderate to severe) pain of 55%. Most importantly, results will be replicated in the additional study participants, as the total number of patients included in the study will be 10 000. In addition, we will use cohorts of our collaborators for replication purposes.
Statistical analysis
The key objective is to identify genetic risk factors that can predict development of acute or chronic postoperative pain and validate previously reported SNPs. A GWA approach will be used as the main analysis. Phenotype data and DNA will be used to identify genetic factors. We will use 5000 patients for the discovery of genetic variants. Samples will be genotyped with the Infinium Global Screening Array (Illumina). Preimputation quality control, principal component analyses and imputation will follow the RICOPILI pipeline.61 Potential confounding by ethnic origin will be corrected by principal component analyses. The 1000 Genomes reference panel will be used for imputation, followed by postimputation quality control in PLINK.62 Associations between SNPs and the presence of acute or chronic pain will be performed using cutting-edge methods when data collection is finished. Results will be replicated to ensure validity. SNPs that can be validated will be included in the prediction model described below.
Secondary objectives include identifying other potential risk factors for acute and chronic postoperative pain. Therefore, a univariate association of each potential predictor will be calculated and tested in a multivariable regression model. We will use a least absolute shrinkage and selection operator (LASSO) regression. Shrinkage is where data values are shrunk towards a central point, like the mean. LASSO is a regression analysis method that performs both variable selection and regularisation to enhance the prediction accuracy and interpretability of the statistical model it produces. After identifying these risk factors, a prediction rule will be created for (moderate to severe) acute and chronic postoperative pain. Based on this prediction rule, a simple, clinically easy applicable tool will be developed to allow clinical use for the stratification of patients. The predictive performance will be studied in another cohort of patients to test whether the rule is generalisable across time and place. Because it appears from the literature that acute and chronic pain are correlated after surgery, additional correlation analysis will be performed to investigate this correlation in the data.
Similar approaches will be followed to identify the clinical and genetic factors that predict pharmacological pain relief. For some pain medicines, genes that impact pain relief are already known (eg, CYP2D6 and morphine). We will first investigate those genes to see if these variants indeed contribute to pharmacological pain relief differences.
Ethics and dissemination
The study will be conducted according to the principles of the Declaration of Helsinki version 2013 and in accordance with the Medical Research Involving Human Subjects Act and Good Clinical Practice. The study was approved by the local ethics committee for human research in Nijmegen (Medical Review Ethics Committee Region Arnhem-Nijmegen, authorisation number: 2012/117). This study was registered on ClinicalTrials.gov (NCT02383342).
The privacy of the participants is guaranteed by storing encrypted data. Every participant will receive a pseudo-anonymous study number. No identifying data is recorded within the meaning of the law. The key is only accessible to the study team and monitors. Data and material will only be used in coded form within possible collaborations.
The results of this study will be made available through peer-reviewed scientific journals and presentations at relevant conferences. After a thorough evaluation, decisions will be made regarding including the identified risk factors and constructed prediction models into clinical guidelines, thus facilitating personalised postoperative pain management.
Discussion
This cohort will be a large prospective study to identify risk factors for postoperative pain and to build and evaluate dedicated prediction models for postoperative pain in surgical patients. In addition, the comprehensive information collected in this study will also enable us to answer other research questions regarding postoperative pain, such as the relationships between acute and chronic postoperative pain development. Eventually, these results will be applied in the clinical settings to improve the quality of life for patients who develop postoperative pain.
The strengths of this study are that we will include all elective major operations rather than limiting to one specific operation as in previous studies,32 which allows us to investigate the shared genetic background of postoperative pain in different operations. Furthermore, as there are discrepancies in pain intensity scores understanding63 and pain management decisions63 64 between patients and caregivers, the patient’s perspective should be respected and assessed for pain evaluation and management.65 66 Therefore, pain assessment will be conducted by patients themselves (patient-reported outcomes) rather than professionals in this study, leading to a more comprehensive outcome assessment and interpretation.67 Moreover, the single-use of NRS might be inadequate for patients’ pain experience evaluation and pain management decisions.66 68 69 Thus, another strength of this cohort is that the experience of pain will be estimated by multidimensional measurements focusing on patients’ overall functionality rather than merely an NRS pain score. In addition, the comprehensively collected information for postoperative pain in this cohort also empowers analysis that cannot be performed in large-scale registry data (eg, UK Biobank) as such phenotype data are not available in those datasets. The data collected in this cohort will also enable additional research using conventional and cutting-edge statistical methods like artificial intelligence.
The possible limitations of this study are that we will only investigate DNA variants as biomarkers for pain prediction as our primary research goal. However, other epigenetic,69 70 transcriptomic,70 proteomics71 and metabolic markers72 are also potentially involved in (postoperative) pain development. For instance, recent studies indicate that methylation patterns might predict opioid treatment outcomes.69 70 As the DNA sample of patients is accessible, we will be able to characterise the multiomics biomarker signatures of postoperative pain in future researches, such as investigating the association between epigenetic changes and postoperative pain. In addition, when prediction tools are applied in clinical settings, the sensitivity and specificity of prediction tools are crucial to evaluate their adequacy and usefulness.73 Although the measurement tools used in prediction models are well-validated and verified (see methods), our findings could still be subject to false positive or negative errors because all measurement tools have limitations. Furthermore, chronic pain assessment is more complex than acute pain,74 and GWAS findings are sometimes incidental.75 We will consider seeking other available cohorts for validation and applying other statistical methods to validate our findings in future studies, such as polygenic risk scores.76 Another potential limitation is that loss of follow-up of patients might result in lower patient numbers than expected. Despite this potential concern, we still expect a sufficient sample size as additional centres will start patient inclusion, and the measurements are mainly from patient-reported outcomes via digital follow-up.
Identifying the genetic background of postoperative pain development may give valuable insights into the mechanisms underlying the relationship between postoperative pain and complications after surgery. This may open the way to identify new targets for treatment and potentially simplify the risk profiling assay for future use, yielding a simpler, more accurate and cost-efficient assay or product. The contribution of improved prevention and treatment of pain after surgery will benefit many patients undergoing surgery and society by decreasing healthcare service costs.
Trial status
Patient recruitment is expected to continue until 2025. Recruitment has already started in Radboud university medical centre, with more than 500 patients recruited as of October 2021. National and international collaborations will be greatly accepted after careful consideration.
Supplementary Material
Acknowledgments
SL was supported by China Scholarship Council (CSC) Grant number 201908130179.
Footnotes
Contributors: RLMvB, MJHC and KV are responsible for overall planning and execution, formulation and evolution of overarching research goals and aims, development and design of the methodology. RLMvB, MJHC and SASvdH will be responsible for project management and coordination responsibility. Analyses and data visualisation will be conducted by SL, RLMvB and MJHC. SL prepared the draft of the manuscript, and all authors critically revised the manuscript.
Funding: Departmental funding covers the costs of this study (grant number: N/A). We aim to apply for extra grants to cover the potential cost of including more patients and the cost of databank maintenance.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain 2012;13:715–24. 10.1016/j.jpain.2012.03.009 [DOI] [PubMed] [Google Scholar]
- 2.Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth 2002;89:409–23. 10.1093/bja/89.3.409 [DOI] [PubMed] [Google Scholar]
- 3.Sommer M, de Rijke JM, van Kleef M, et al. The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur J Anaesthesiol 2008;25:267–74. 10.1017/S0265021507003031 [DOI] [PubMed] [Google Scholar]
- 4.Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 2017;10:2287–98. 10.2147/JPR.S144066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Boekel RLM, Warlé MC, Nielen RGC, et al. Relationship between postoperative pain and overall 30-day complications in a broad surgical population: an observational study. Ann Surg 2019;269:856–65. 10.1097/SLA.0000000000002583 [DOI] [PubMed] [Google Scholar]
- 6.Peters CL, Shirley B, Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty 2006;21:132–8. 10.1016/j.arth.2006.04.017 [DOI] [PubMed] [Google Scholar]
- 7.Regenbogen SE, Mullard AJ, Peters N, et al. Hospital analgesia practices and patient-reported pain after colorectal resection. Ann Surg 2016;264:1044–50. 10.1097/SLA.0000000000001541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katz J, Jackson M, Kavanagh BP, et al. Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. Clin J Pain 1996;12:50–5. 10.1097/00002508-199603000-00009 [DOI] [PubMed] [Google Scholar]
- 9.Schug SA, Lavand'homme P, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain 2019;160:45–52. 10.1097/j.pain.0000000000001413 [DOI] [PubMed] [Google Scholar]
- 10.Apfelbaum JL, Chen C, Mehta SS, et al. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 2003;97:534–40. 10.1213/01.ANE.0000068822.10113.9E [DOI] [PubMed] [Google Scholar]
- 11.Meissner W, Coluzzi F, Fletcher D, et al. Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin 2015;31:2131–43. 10.1185/03007995.2015.1092122 [DOI] [PubMed] [Google Scholar]
- 12.Zimberg SE. Reducing pain and costs with innovative postoperative pain management. Manag Care Q 2003;11:34–6. [PubMed] [Google Scholar]
- 13.Morrison SR, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain 2003;103:303–11. 10.1016/S0304-3959(02)00458-X [DOI] [PubMed] [Google Scholar]
- 14.Zoucas E, Lydrup M-L. Hospital costs associated with surgical morbidity after elective colorectal procedures: a retrospective observational cohort study in 530 patients. Patient Saf Surg 2014;8:2. 10.1186/1754-9493-8-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Encinosa WE, Hellinger FJ. The impact of medical errors on ninety-day costs and outcomes: an examination of surgical patients. Health Serv Res 2008;43:2067–85. 10.1111/j.1475-6773.2008.00882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med 2010;11:1859–71. 10.1111/j.1526-4637.2010.00983.x [DOI] [PubMed] [Google Scholar]
- 17.Glare P, Aubrey KR, Myles PS. Transition from acute to chronic pain after surgery. Lancet 2019;393:1537–46. 10.1016/S0140-6736(19)30352-6 [DOI] [PubMed] [Google Scholar]
- 18.Yang MMH, Hartley RL, Leung AA, et al. Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ Open 2019;9:e025091. 10.1136/bmjopen-2018-025091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalkman JC, Visser K, Moen J, et al. Preoperative prediction of severe postoperative pain. Pain 2003;105:415–23. 10.1016/S0304-3959(03)00252-5 [DOI] [PubMed] [Google Scholar]
- 20.Janssen KJM, Kalkman CJ, Grobbee DE, et al. The risk of severe postoperative pain: modification and validation of a clinical prediction rule. Anesth Analg 2008;107:1330–9. 10.1213/ane.0b013e31818227da [DOI] [PubMed] [Google Scholar]
- 21.Hoofwijk DMN, van Reij RRI, Rutten BPF, et al. Genetic polymorphisms and prediction of chronic post-surgical pain after hysterectomy-a subgroup analysis of a multicenter cohort study. Acta Anaesthesiol Scand 2019;63:1063–73. 10.1111/aas.13413 [DOI] [PubMed] [Google Scholar]
- 22.Althaus A, Hinrichs-Rocker A, Chapman R, et al. Development of a risk index for the prediction of chronic post-surgical pain. Eur J Pain 2012;16:901–10. 10.1002/j.1532-2149.2011.00090.x [DOI] [PubMed] [Google Scholar]
- 23.Montes A, Roca G, Cantillo J, et al. Presurgical risk model for chronic postsurgical pain based on 6 clinical predictors: a prospective external validation. Pain 2020;161:2611–8. 10.1097/j.pain.0000000000001945 [DOI] [PubMed] [Google Scholar]
- 24.Montes A, Roca G, Sabate S, et al. Genetic and clinical factors associated with chronic postsurgical pain after hernia repair, hysterectomy, and thoracotomy: a two-year multicenter cohort study. Anesthesiology 2015;122:1123–41. 10.1097/ALN.0000000000000611 [DOI] [PubMed] [Google Scholar]
- 25.Mauck M, Van de Ven T, Shaw AD. Epigenetics of chronic pain after thoracic surgery. Curr Opin Anaesthesiol 2014;27:1–5. 10.1097/ACO.0000000000000030 [DOI] [PubMed] [Google Scholar]
- 26.van Reij RRI, Joosten EAJ, van den Hoogen NJ. Dopaminergic neurotransmission and genetic variation in chronification of post-surgical pain. Br J Anaesth 2019;123:853–64. 10.1016/j.bja.2019.07.028 [DOI] [PubMed] [Google Scholar]
- 27.De Gregori M, Diatchenko L, Belfer I, et al. OPRM1 receptor as new biomarker to help the prediction of post mastectomy pain and recurrence in breast cancer. Minerva Anestesiol 2015;81:894–900. [PubMed] [Google Scholar]
- 28.Hoofwijk DMN, van Reij RRI, Rutten BP, et al. Genetic polymorphisms and their association with the prevalence and severity of chronic postsurgical pain: a systematic review. Br J Anaesth 2016;117:708–19. 10.1093/bja/aew378 [DOI] [PubMed] [Google Scholar]
- 29.Kim H, Clark D, Dionne RA. Genetic contributions to clinical pain and analgesia: avoiding pitfalls in genetic research. J Pain 2009;10:663–93. 10.1016/j.jpain.2009.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mueller C, Klega A, Buchholz H-G, et al. Basal opioid receptor binding is associated with differences in sensory perception in healthy human subjects: a [18F]diprenorphine PET study. Neuroimage 2010;49:731–7. 10.1016/j.neuroimage.2009.08.033 [DOI] [PubMed] [Google Scholar]
- 31.van Reij RRI, Hoofwijk DMN, Rutten BPF, et al. The association between genome-wide polymorphisms and chronic postoperative pain: a prospective observational study. Anaesthesia 2020;75 Suppl 1:e111–20. 10.1111/anae.14832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warner SC, van Meurs JB, Schiphof D, et al. Genome-wide association scan of neuropathic pain symptoms post total joint replacement highlights a variant in the protein-kinase C gene. Eur J Hum Genet 2017;25:446–51. 10.1038/ejhg.2016.196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zubieta J-K, Heitzeg MM, Smith YR, et al. COMT Val158Met genotype affects mu-opioid neurotransmitter responses to a pain stressor. Science 2003;299:1240–3. 10.1126/science.1078546 [DOI] [PubMed] [Google Scholar]
- 34.Rakvåg TT, Klepstad P, Baar C, et al. The Val158Met polymorphism of the human catechol-O-methyltransferase (COMT) gene may influence morphine requirements in cancer pain patients. Pain 2005;116:73–8. 10.1016/j.pain.2005.03.032 [DOI] [PubMed] [Google Scholar]
- 35.Reyes-Gibby CC, Shete S, Rakvåg T, et al. Exploring joint effects of genes and the clinical efficacy of morphine for cancer pain: OPRM1 and COMT gene. Pain 2007;130:25–30. 10.1016/j.pain.2006.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Owusu Obeng A, Hamadeh I, Smith M. Review of opioid pharmacogenetics and considerations for pain management. Pharmacotherapy 2017;37:1105–21. 10.1002/phar.1986 [DOI] [PubMed] [Google Scholar]
- 37.De Gregori M, Diatchenko L, Ingelmo PM, et al. Human genetic variability contributes to postoperative morphine consumption. J Pain 2016;17:628–36. 10.1016/j.jpain.2016.02.003 [DOI] [PubMed] [Google Scholar]
- 38.Haller G, Bampoe S, Cook T, et al. Systematic review and consensus definitions for the standardised endpoints in perioperative medicine initiative: clinical indicators. Br J Anaesth 2019;123:228–37. 10.1016/j.bja.2019.04.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pogatzki-Zahn E, Schnabel K, Kaiser U. Patient-reported outcome measures for acute and chronic pain: current knowledge and future directions. Curr Opin Anaesthesiol 2019;32:616–22. 10.1097/ACO.0000000000000780 [DOI] [PubMed] [Google Scholar]
- 40.Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med 1999;130:515–24. 10.7326/0003-4819-130-6-199903160-00016 [DOI] [PubMed] [Google Scholar]
- 41.Reilly BM, Evans AT. Translating clinical research into clinical practice: impact of using prediction rules to make decisions. Ann Intern Med 2006;144:201–9. 10.7326/0003-4819-144-3-200602070-00009 [DOI] [PubMed] [Google Scholar]
- 42.Altman DG, Royston P. What do we mean by validating a prognostic model? Stat Med 2000;19:453–73. [DOI] [PubMed] [Google Scholar]
- 43.Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996;15:361–87. [DOI] [PubMed] [Google Scholar]
- 44.Castor EDC. Castor electronic data capture 2019. Available: https://castoredc.com [Accessed 28 Aug 2019].
- 45.Soer R, Köke AJA, Vroomen PCAJ, et al. Extensive validation of the pain disability index in 3 groups of patients with musculoskeletal pain. Spine 2013;38:E562–8. 10.1097/BRS.0b013e31828af21f [DOI] [PubMed] [Google Scholar]
- 46.Tait RC, Pollard CA, Margolis RB, et al. The pain disability index: psychometric and validity data. Arch Phys Med Rehabil 1987;68:438–41. [PubMed] [Google Scholar]
- 47.Moerman N, van Dam FS, Muller MJ, et al. The Amsterdam preoperative anxiety and information scale (APAIS). Anesth Analg 1996;82:445–51. 10.1097/00000539-199603000-00002 [DOI] [PubMed] [Google Scholar]
- 48.Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995;7:524–32. 10.1037/1040-3590.7.4.524 [DOI] [Google Scholar]
- 49.Ruscheweyh R, Marziniak M, Stumpenhorst F, et al. Pain sensitivity can be assessed by self-rating: development and validation of the pain sensitivity questionnaire. Pain 2009;146:65–74. 10.1016/j.pain.2009.06.020 [DOI] [PubMed] [Google Scholar]
- 50.Van Boekel RLM, Timmerman H, Bronkhorst EM, et al. Translation, cross-cultural adaptation, and validation of the pain sensitivity questionnaire in dutch healthy volunteers. Pain Res Manag 2020;2020:1–10. 10.1155/2020/1050935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rush AJ, Giles DE, Schlesser MA, et al. The inventory for depressive symptomatology (IDS): preliminary findings. Psychiatry Res 1986;18:65–87. 10.1016/0165-1781(86)90060-0 [DOI] [PubMed] [Google Scholar]
- 52.Rush AJ, Gullion CM, Basco MR, et al. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol Med 1996;26:477–86. 10.1017/S0033291700035558 [DOI] [PubMed] [Google Scholar]
- 53.Rothaug J, Zaslansky R, Schwenkglenks M, et al. Patients' perception of postoperative pain management: validation of the international pain outcomes (ipo) questionnaire. J Pain 2013;14:1361–70. 10.1016/j.jpain.2013.05.016 [DOI] [PubMed] [Google Scholar]
- 54.Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap 1994;23:129–38. [PubMed] [Google Scholar]
- 55.Dindo D, Clavien P-A. What is a surgical complication? World J Surg 2008;32:939–41. 10.1007/s00268-008-9584-y [DOI] [PubMed] [Google Scholar]
- 56.Gerbershagen HJ, Rothaug J, Kalkman CJ, et al. Determination of moderate-to-severe postoperative pain on the numeric rating scale: a cut-off point analysis applying four different methods. Br J Anaesth 2011;107:619–26. 10.1093/bja/aer195 [DOI] [PubMed] [Google Scholar]
- 57.Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain 2019;160:19–27. 10.1097/j.pain.0000000000001384 [DOI] [PubMed] [Google Scholar]
- 58.Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth 2008;101:77–86. 10.1093/bja/aen099 [DOI] [PubMed] [Google Scholar]
- 59.Werner MU, Kongsgaard UE. I. defining persistent post-surgical pain: is an update required? Br J Anaesth 2014;113:1–4. 10.1093/bja/aeu012 [DOI] [PubMed] [Google Scholar]
- 60.Purcell S, Cherny SS, Sham PC. Genetic power calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics 2003;19:149–50. 10.1093/bioinformatics/19.1.149 [DOI] [PubMed] [Google Scholar]
- 61.Lam M, Awasthi S, Watson HJ, et al. Ricopili: rapid imputation for consortias pipeline. Bioinformatics 2020;36:930–3. 10.1093/bioinformatics/btz633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Purcell S, Neale B, Todd-Brown K, et al. Plink: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007;81:559–75. 10.1086/519795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van Dijk JFM, van Wijck AJM, Kappen TH, et al. Postoperative pain assessment based on numeric ratings is not the same for patients and professionals: a cross-sectional study. Int J Nurs Stud 2012;49:65–71. 10.1016/j.ijnurstu.2011.07.009 [DOI] [PubMed] [Google Scholar]
- 64.Harting B, Johnson T, Abrams R, et al. An exploratory analysis of the correlation of pain scores, patient satisfaction with relief from pain, and a new measure of pain control on the total dose of opioids in pain care. Qual Manag Health Care 2013;22:322–6. 10.1097/QMH.0000000000000009 [DOI] [PubMed] [Google Scholar]
- 65.Raja SN, Carr DB, Cohen M, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 2020;161:1976–82. 10.1097/j.pain.0000000000001939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.van Boekel RLM, Vissers KCP, van der Sande R, et al. Moving beyond pain scores: multidimensional pain assessment is essential for adequate pain management after surgery. PLoS One 2017;12:e0177345. 10.1371/journal.pone.0177345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weldring T, Smith SMS. Patient-reported outcomes (pros) and patient-reported outcome measures (PROMs). Health Serv Insights 2013;6:61–8. 10.4137/HSI.S11093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sloman R, Wruble AW, Rosen G, et al. Determination of clinically meaningful levels of pain reduction in patients experiencing acute postoperative pain. Pain Manag Nurs 2006;7:153–8. 10.1016/j.pmn.2006.09.001 [DOI] [PubMed] [Google Scholar]
- 69.Clark CW, Yang JC, Tsui S-L, et al. Unidimensional pain rating scales: a multidimensional affect and pain survey (maps) analysis of what they really measure. Pain 2002;98:241–7. 10.1016/S0304-3959(01)00474-2 [DOI] [PubMed] [Google Scholar]
- 70.Dorsey SG, Renn CL, Griffioen M, et al. Whole blood transcriptomic profiles can differentiate vulnerability to chronic low back pain. PLoS One 2019;14:e0216539. 10.1371/journal.pone.0216539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Van Der Heijden H, Fatou B, Sibai D, et al. Proteomics based markers of clinical pain severity in juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2022;20:3. 10.1186/s12969-022-00662-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jha MK, Song GJ, Lee MG, et al. Metabolic connection of inflammatory pain: pivotal role of a pyruvate dehydrogenase kinase-pyruvate dehydrogenase-lactic acid axis. J Neurosci 2015;35:14353–69. 10.1523/JNEUROSCI.1910-15.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Trevethan R, Sensitivity TR. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health 2017;5:307. 10.3389/fpubh.2017.00307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fillingim RB, Loeser JD, Baron R, et al. Assessment of chronic pain: domains, methods, and mechanisms. J Pain 2016;17:T10–20. 10.1016/j.jpain.2015.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ioannidis JPA. Non-replication and inconsistency in the genome-wide association setting. Hum Hered 2007;64:203–13. 10.1159/000103512 [DOI] [PubMed] [Google Scholar]
- 76.van Reij RRI, Voncken JW, Joosten EAJ, et al. Polygenic risk scores indicates genetic overlap between peripheral pain syndromes and chronic postsurgical pain. Neurogenetics 2020;21:205–15. 10.1007/s10048-020-00614-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-066134supp001.pdf (404.8KB, pdf)