Abstract
STUDY QUESTION
How did the first two coronavirus disease 2019 (COVID-19) waves affect fertility rates in the USA?
SUMMARY ANSWER
States differed widely in how their fertility rates changed following the COVID-19 outbreak and these changes were influenced more by state-level economic, racial, political, and social factors than by COVID-19 wave severity.
WHAT IS KNOWN ALREADY
The outbreak of the COVID-19 pandemic contributed to already declining fertility rates in the USA, but not equally across states. Identifying drivers of differential changes in fertility rates can help explain variations in demographic shifts across states in the USA and motivate policies that support families in general, not only during crises.
STUDY DESIGN, SIZE, DURATION
This is an ecological study using state-level data from 50 US states and the District of Columbia (n = 51). The study period extends from 2020 to 2021 with historical data from 2016 to 2019. We identified Wave 1 as the first apex for each state after February 2020 and Wave 2 as the second apex, during Fall/Winter 2020–2021.
PARTICIPANTS/MATERIALS, SETTING, METHODS
State-level COVID-19 wave severity, defined as case acceleration during each 3-month COVID-19 wave (cases/100 000 population/month), was derived from 7-day weekly moving average COVID-19 case rates from the US Centers for Disease Control and Prevention (CDC). State-level fertility rate changes (change in average monthly fertility rate/100 000 women of reproductive age (WRA)/year) were derived from the CDC Bureau of Vital Statistics and from 2020 US Census and University of Virginia 2021 population estimates 9 months after each COVID-19 wave. We performed univariate analyses to describe national and state-level fertility rate changes following each wave, and simple and multivariable linear regression analyses to assess the relation of COVID-19 wave severity and other state-level characteristics with fertility rate changes.
MAIN RESULTS AND THE ROLE OF CHANCE
Nationwide, fertility dropped by 17.5 births/month/100 000 WRA/year following Wave 1 and 9.2 births/month/100 000 WRA/year following Wave 2. The declines following Wave 1 were largest among majority-Democrat, more non-White states where people practiced greater social distancing. Greater COVID-19 wave severity was associated with steeper fertility rate decline post-Wave 1 in simple regression, but the association was attenuated when adjusted for other covariates. Adjusting for the economic impact of the pandemic (hypothesized mediator) also attenuated the effect. There was no relation between COVID-19 wave severity and fertility rate change following Wave 2.
LIMITATIONS, REASONS FOR CAUTION
Our study harnesses state-level data so individual-level conclusions cannot be inferred. There may be residual confounding in our multivariable regression and we were underpowered to detect some effects.
WIDER IMPLICATIONS OF THE FINDINGS
The COVID-19 pandemic initially impacted the national fertility rate but, overall, the fertility rate rebounded to the pre-pandemic level following Wave 2. Consistent with prior literature, COVID-19 wave severity did not appear to predict fertility rate change. Economic, racial, political, and social factors influenced state-specific fertility rates during the pandemic more than the severity of the outbreak alone. Future studies in other countries should also consider whether these factors account for internal heterogeneity when examining the impact of the COVID-19 pandemic and other crises on fertility.
STUDY FUNDING/COMPETING INTEREST(S)
L.G.K. received funding from the National Institute of Environmental Health Sciences (R00ES030403), M.C. from the National Science Foundation Graduate Research Fellowship Program (20-A0-00-1005789), and M.L. and E.S. from the National Institute of Environmental Health Sciences (R01ES032808). None of the authors have competing interests.
TRIAL REGISTRATION NUMBER
N/A.
Keywords: fertility, COVID-19, pandemic, fertility trends, birth rates, coronavirus disease 2019, severe acute respiratory syndrome coronavirus 2, ecological study, US state analysis, social determinants
Introduction
Few events in recent history have disrupted society to the extent of the coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2. Outside of changes to everyday life and activities, reproductive behavior changed as well, with steep reductions in the desire to become pregnant shortly after the start of the pandemic (Seltzer, 2019; Lindberg et al., 2020; Cohen, 2021; Kahn et al., 2021; Lin et al., 2021; Lindberg et al., 2021; Morse, 2021; Kearney et al., 2022). The result in the USA was a precipitous drop in births: a study examining one-third of all births in New York City found a 20% decrease in births 9 months after the March–June 2020 COVID-19 wave compared with the average over the prior 4 years (McLaren et al., 2021); another study showed declines in births 9 months following the initial COVID-19 wave in nine states (Cohen, 2021); and National Center for Health Statistics data revealed a reduction in births in December 2020 and January 2021 (Morse, 2021). However, it is unknown if fertility rates declined uniformly across the USA or varied by state-level factors, or if they remained depressed over time.
Increasing COVID-19 cases could influence fertility rates by reducing pregnancy-intention via heightened pandemic anxiety, pandemic-related restrictions, and/or economic hardship. Economic hardship has been shown to be related to reduced fertility rates in the context of both the 2008 recession (Sobotka et al., 2011) and the Great Depression (Schneider, 2015; De Geyter, 2022). Without overarching federal policies, the public health response to the COVID-19 outbreak was dependent on individual states. Thus, residents in each state likely experienced factors, such as pandemic-related anxiety, restrictions, and economic stress, differently depending on the severity of the epidemic in their locale and their state government’s policies. In addition to differing in their pandemic response, states already differ widely in terms of demographic and economic features, which are known drivers of fertility rates (Colleran and Snopkowski, 2018; Marcén et al., 2018; Hellstrand et al., 2020; Aitken, 2022).
Other studies have demonstrated that differences in both pregnancy intention and births following the COVID-19 outbreak were not consistent across countries and varied according to both COVID-19 severity and demography. For example, an Australian study found that women planning pregnancy only reported higher psychological distress than women not planning pregnancy in locations with high COVID-19 restrictions and viral transmission (Schoenaker et al., 2022). A Japanese study found that decreases in births following the first state of emergency were greater in urban than rural areas (Ghaznavi et al., 2022). Existing studies on fertility rate changes following the COVID-19 pandemic in the USA have not accounted for between-state variation in their analyses (Koenig et al., 2022), nor have European studies that have focused only on the country level (De Geyter et al., 2022).
Given the lack of US state-specific fertility rate research in the context of COVID-19 and evidence suggesting that demographic and economic features may be important determinants of both the COVID-19 experience and fertility rates (Adolph et al., 2022; Erwin et al., 2021; Jha, 2020; Neelon et al., 2021; Rodriguez et al., 2022), we chose to examine US states individually. We hypothesized that in the first wave of the outbreak, COVID-19 wave severity, operationalized as the case acceleration rate, would be inversely associated with annual change in monthly fertility rate, with a particularly strong effect in states that were more liberal politically and implemented more stringent COVID-19 policies. We considered that economic disruption, which has historically been linked to reduced fertility rates (Clark, 2012; Sweeney and Raley, 2014; Buckles et al., 2020; Bailey et al., 2022), might mediate this association. We also hypothesized that COVID-19 wave severity would not correlate as strongly with fertility rate change following the second wave, as society would have developed some tolerance for pandemic-related anxiety and economic resilience owing to the distribution of government stimulus checks.
Materials and methods
Study design
This ecological study examines associations between the severity of the first two COVID-19 waves and changes in monthly fertility rates in all 50 US states and Washington, DC (‘states’) 9 months after each wave. We chose to examine waves as opposed to COVID-19 rates continuously over time because waves are periods when we might observe the most acute pandemic effects on fertility. Also, restricting to waves removes concerns about many time-varying confounders. There is no definitive method to operationalize a pandemic wave in the literature (Hale et al., 2021; Zhang et al., 2021). However, it is generally accepted that a wave is a period of substantial and/or sustained upward and downward movement of some epidemic metric that is not attributable to random error or noise (Hale et al., 2021; Zhang et al., 2021). We were restricted to considering entire calendar months, as publicly available fertility rate data only exist in this format; therefore, we could not use exact dates to define our waves. Instead, we defined waves as 3-month windows in which cases increased, peaked, then declined. Case rates were defined as the 7-day moving average of COVID-19 cases/100 000 population reported by the US Centers for Disease Control and Prevention (CDC) (CDC, 2023). Using graphs of the 7-day moving average of case rates across time, we identified the apex of each wave for each state. We identified Wave 1 as the first apex for each state after February 2020 and Wave 2 as the second apex, during Fall/Winter 2020–2021. Three coders (S.A., M.C., and E.S.) applied this method of wave identification to all states and had an interrater reliability of 0.85 for Wave 1 and 0.97 for Wave 2. Discrepancies were resolved by consensus.
Since we were restricted to using calendar months for the monthly fertility rate data, if the peak occurred at either end of a calendar month we had to decide if that counted as the peak month. Per our definition of a pandemic wave, we sought to make sure the sustained increase leading up to the peak was captured in the 3-month wave identified for each state. We found that if the peak case rate was reached before the 10th of the month, the sustained increase most often began 2 months prior, so rather than assigning that month as the peak month, we assigned the month prior as the peak month.
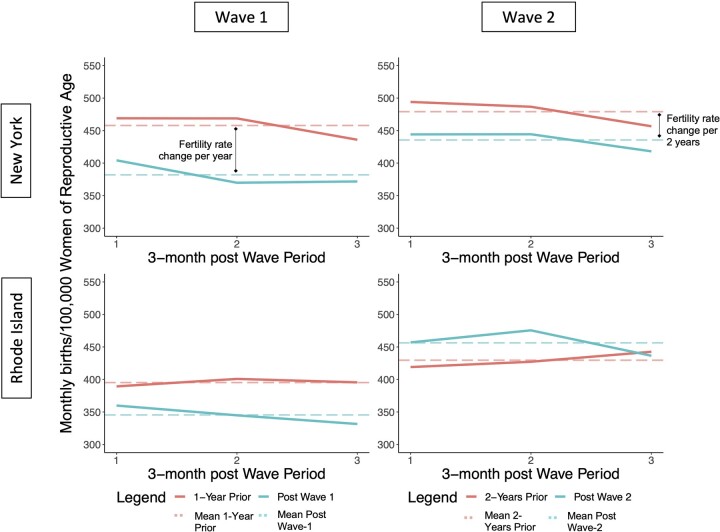
Outcome
Our outcome was the annual change in average monthly fertility rate (change in number of births/month/100 000 women of reproductive age (15–44 years) (WRA)/year) 9 months following the first two COVID-19 waves in each state (the average gestational length). We obtained birth data from the CDC Bureau of Vital Statistics and divided each month’s total by the number of WRA for that state and year, obtained from the US Census (Ellington et al., 2020). Census numbers of WRA were not available for 2021, so we used projections of WRA for 2021 from the University of Virginia (University of Virginia Weldon Cooper Center DRG, 2018). For Wave 1, we calculated the difference between fertility rates 9 months following Wave 1 and the same months in the year prior, to account for seasonal fluctuation of fertility rates. Since the pandemic had already impacted fertility rates by late 2020, for Wave 2 we compared fertility rates to the corresponding months 2 years prior and divided the result by two. Figure 1 illustrates this process for New York and Rhode Island for each wave. We also calculated pre-pandemic (secular) fertility rate trends by averaging annual changes in average monthly fertility rates across 2016–2019.
Figure 1.
Calculation of annual change in average monthly fertility rate for New York and Rhode Island following COVID-19 waves. Each panel represents the fertility rate (average monthly births/100 000 women of reproductive age) in the 9 months following each coronavirus disease 2019 (COVID-19) wave compared to the fertility rate in the same months in previous years (1 year prior for Wave 1, 2 years prior for Wave 2). The dotted lines show the mean fertility rate for each period. The vertical black lines indicate the annual (Wave 1) or biannual (Wave 2) average monthly fertility rate change.
Exposure
Our primary exposure was the acceleration of COVID-19 cases during each wave, which we refer to as COVID-19 wave severity, defined as the increase in cases/100 000 residents/month determined by the difference in the 7-day moving average statewide COVID-19 case rate between the wave’s peak and the same date a month prior. For Wave 2, several states’ waves had two peaks; in those cases, we selected the first peak of the wave. We chose wave severity as a proxy for COVID-19 anxiety that might affect pregnancy intention rather than death or hospitalization rates because we aimed to capture the fear around the spread of COVID-19, not the consequences of the virus.
Covariates
Potential covariates included other factors that might be associated with both our exposure, outcome, and/or hypothesized mediators (Supplementary Fig. S1). We considered two variables as proxies for how seriously states’ populations may have taken the risk posed by the pandemic. One was political leaning of the state, operationalized as the percentage that voted Republican in the 2020 presidential election. Political leaning was strongly linked to how importantly individuals rated the COVID-19 outbreak in relation to the 2020 election, according to a Pew Research Center poll (Dunn, 2020). Political leaning of a state might also correlate with a state’s government response to the COVID-19 pandemic. Because of the ecological nature of this study, these two effects cannot be disentangled. The other variable we considered was lockdown-related changes in behavior, operationalized as a Social Distancing Index (SDI; 0–100) derived by researchers at the University of Maryland based on data from mobile devices (Zhang et al., 2020). As with political leaning, behavioral changes in social distancing may reflect how seriously individuals in a state responded to COVID-19 restrictions as well as the prevalence and intensity of restrictions imposed or recommended by state authorities. Demographic variables included states’ racial and ethnic diversity (percentage non-White, percent Hispanic), age structure (percentage ≥65 years), rurality (percentage living in a rural area), and educational attainment (percentage ≥Associate degree) (U.S. Census Bureau, 2022). Economic variables included states’ poverty rate, income inequality ratio, affordable housing units, and employment change at the start of the pandemic. We also evaluated whether a state voted for Medicaid expansion in 2020 (Foundation KF, 2022). Finally, we considered when within each wave a particular state’s peak occurred (Spring versus Summer for Wave 1, Fall versus Winter for Wave 2).
We hypothesized that economic impact of the pandemic and reduced pregnancy intention might mediate the relation between COVID-19 wave severity and annual fertility rate change. While we were unable to capture pregnancy intention for the purposes this study, we did attempt to approximate the economic impact of the pandemic at the state level through employment change. Employment change was calculated as the difference in employment rate from the end of February 2020 to the end of April 2020, when the most dramatic change in employment occurred across all states following the outbreak (Marazzi, 2022) (Supplementary Table SI provides details on data sources).
Statistical methods
We calculated the annual change in average monthly fertility rates for all states by comparing average monthly fertility rates 9 months following Wave 1 and Wave 2 with those 1 year and 2 years prior, respectively. We also compared observed fertility rates 9 months following each wave with expected rates extrapolated from pre-COVID (2016–2019) secular trends. We combined state-level data to create national averages by weighting each state by the size of its population of WRA. We conducted analysis of variance to compare average fertility rate change across categories of our main exposure and potential covariates. Finally, we conducted simple and covariate-adjusted linear regression analyses to assess the association between wave severity and fertility rate change separately for each wave. Covariates were selected based on literature review and a directed acyclic graph, with an eye toward avoiding collinearity (Supplementary Fig. S1). Because SDI was not available for the period following Wave 2, we were not able to include it in our models; instead, we included the percentage that voted Republican in 2020, as the two variables were highly correlated (r = −0.74, P < 0.01). Our final covariate set included percentage voted Republican in 2020, percentage non-White, affordable housing units, and wave timing. We performed an exploratory test of our mediation hypothesis by additionally controlling for economic impact of the pandemic in a separate model. To test the hypothesis that politics might moderate the association between COVID-19 wave severity and fertility rate change, we stratified our analyses by states where a majority versus minority voted Republican in 2020. We performed two-tailed significance tests (ɑ = 0.05) and conducted all analyses in R (V4.0.5) (R Core Team, 2022).
Sensitivity analyses
Because the pandemic caused many people to relocate and population movement was not uniform across states, we conducted a sensitivity analysis in which we accounted for state-to-state migration. Using monthly US Postal Service change-of-address request data, we assumed two-thirds of all individuals and households that moved contained a WRA and added or subtracted the appropriate number from each state’s fertility rate denominator. We also tested whether secular trends in fertility rates might explain associations between predictors and fertility rate changes by controlling for states’ pre-pandemic trends in our regression models.
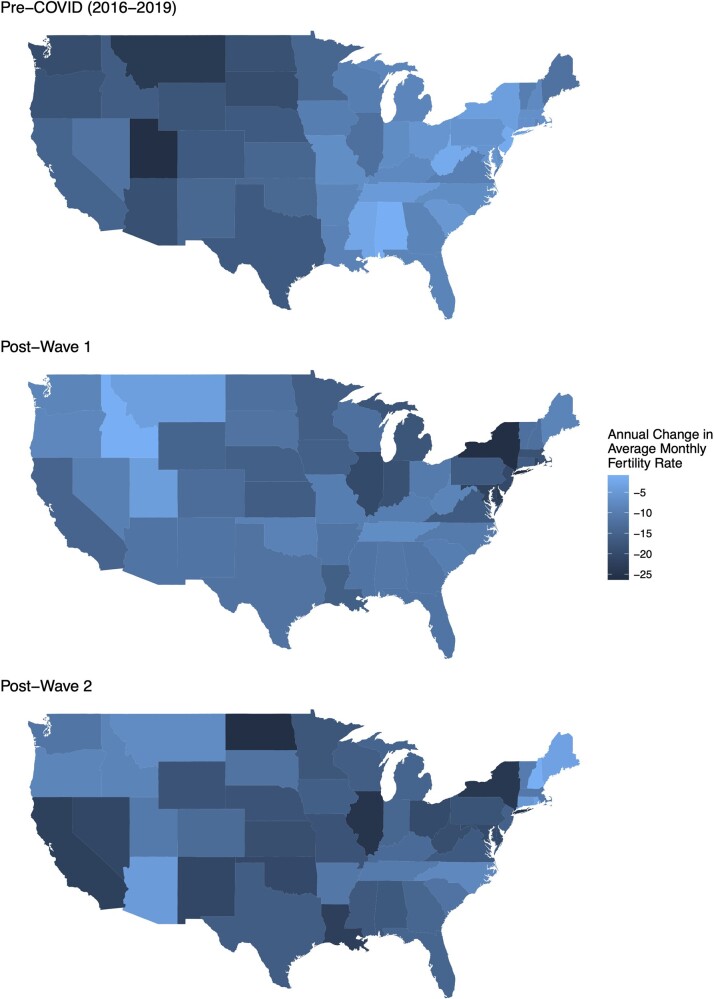
Results
The pre-pandemic (2016–2019) national annual change in average monthly fertility rate was −10.6 births/month/100 000 WRA/year (SD = 5.3; range: −26.3, −0.9), indicating a downward secular trend. Nine months after Wave 1, the annual change was −17.5 births/month/100 000 WRA/year (SD = 23.4; range: −75.9, 46.4), a significant decrease from the pre-pandemic trend (weighted mean difference = −6.92, 95% CI = −13.73, −0.11). Nine months after Wave 2, the annual change was −9.2 births/month/100 000 WRA/year (SD = 8.9; range: −27.2, 17.2), not significantly different from the pre-pandemic trend (weighted mean difference = 1.31, 95% CI = −1.60, 4.22). Following Wave 1 and Wave 2, the expected national fertility rates based on the secular trend would have been 447.0 and 488.9 births/month/100 000 WRA, respectively (Supplementary Table SII presents state-specific rates). The observed rates were 440.1 and 491.5 births/month/100 000 WRA, respectively.
Pre-COVID, all states had declining fertility rates although the magnitude of this decline varied by state (Fig. 2). Four patterns of fertility rate change relative to baseline emerged over the two post-wave periods: declined and recovered beyond pre-COVID trend (n = 12); declined, not yet recovered (n = 12); increased and/or never declined (n = 19); and initially increased, then declined (n = 8) (Supplementary Table SIII and Supplementary Figs S2, S3, and S4).
Figure 2.
State-specific annual fertility rate change for pre-pandemic period, post-Wave 1 and post-Wave 2 for each US state. The top map of the USA shows state-specific annual change in fertility rate (average monthly births/100 000 women of reproductive age) pre-coronavirus disease 2019 (COVID) (averaged from 2016 to 2019). The middle and bottom map shows the state-specific annual change in fertility rate following Wave 1 and Wave 2, respectively.
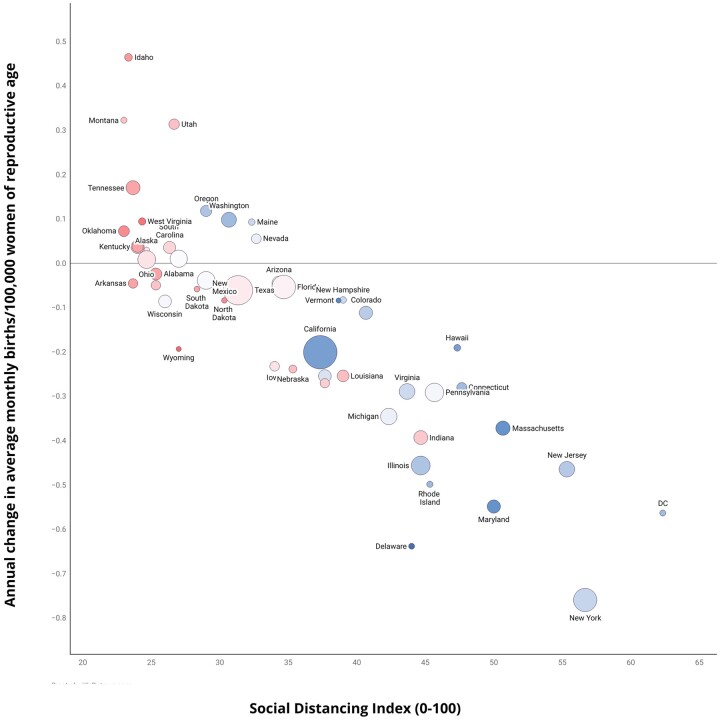
Following Wave 1, states with larger fertility rate declines tended to be more urban and to have greater wave severity, greater proportions of non-White inhabitants and inhabitants with college degrees, higher income inequality, earlier onsets of Wave 1, and larger drops in employment rate at the beginning of the pandemic (Table I, Supplementary Fig. S5). They also had higher proportions of Democratic voters and higher SDIs. Figure 3 illustrates the correlations among SDI, political leaning, and fertility rate change following Wave 1. Following Wave 2, states with larger declines in fertility rate tended to have younger, more non-White populations and have higher income inequality (Table I, Supplementary Fig. S6).
Table I.
US state characteristics by annual change in average monthly fertility rate (births/month/100 000 women of reproductive age/year) following the first two COVID-19 waves.
| Variablea | Category | Wave 1 | Wave 2 |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Wave severityb | High | −22.05 (35.95) | −7.80 (10.64) |
| Low | −11.34 (22.23) | −3.63 (12.55) | |
| Political leaning | Majority Democrat | −24.15 (24.3) | −6.38 (12.69) |
| Majority Republican | −1.44 (19.61) | −7.93 (8.93) | |
| Social Distancing Index | High | −22.05 (35.95) | N/A |
| Low | −11.34 (22.23) | N/A | |
| Percentage non-White | High | −18.26 (25.32) | −11.29 (10.65) |
| Low | −7.98 (23.53) | −3.15 (9.80) | |
| Percentage Hispanic | High | −18.46 (29.85) | −6.91 (10.94) |
| Low | −7.35 (16.74) | −7.38 (11.13) | |
| Percentage 65 years or older | High | −7.81 (20.24) | −4.82 (11.39) |
| Low | −16.37 (27.02) | −8.64 (10.54) | |
| Rurality | Rural | −3.08 (18.22) | −6.45 (10.69) |
| Urban | −23.35 (26.64) | −7.86 (11.35) | |
| Education attainment | High | −20.55 (25.58) | −6.93 (12.46) |
| Low | −4.54 (21.16) | −7.39 (9.16) | |
| Poverty rate | High | −9.17 (22.92) | −8.26 (9.07) |
| Low | −17.02 (26.34) | −5.98 (12.66) | |
| Income inequality ratio | High | −18.53 (24.72) | −8.60 (9.99) |
| Low | −7.28 (23.88) | −5.63 (11.84) | |
| Affordable housing units | High | −10.91 (20.88) | −6.33 (10.54) |
| Low | −15.20 (28.46) | −7.98 (11.47) | |
| Employment change | High | −17.26 (23.42) | −7.52 (8.17) |
| Low | −8.93 (25.71) | −6.78 (13.21) | |
| Medicaid expansion | No | −4.47 (10.73) | −6.12 (5.75) |
| Yes | −15.94 (27.47) | −7.49 (12.25) | |
| Wave timingc | Earlier | −28.88 (20.42) | −8.08 (10.59) |
| Later | 4.83 (15.16) | −6.49 (11.29) |
Continuous variables are split at the median into low and high categories.
Change in 7-day moving average of coronavirus disease 2019 (COVID-19) cases per 100 000 between first and peak month of wave.
Earlier: Spring for Wave 1, Fall for Wave 2; Later: Summer for Wave 2, Winter for Wave 2.
Bolded cells indicate an analysis of variance F-test comparing the means of the two categories had a P-value <0.05. See Supplementary Figs S5 and S6 for full correlation matrices for each wave, respectively.
Figure 3.
Annual fertility rate change in the USA in relation to social distancing index and political leaning following Wave 1. Following Wave 1, fertility rate change is correlated with Social Distancing Index (x-axis) and political leaning (red: Republican, blue; Democrat). Social Distancing Index is a scale from 0 to 100, with higher values indicating greater levels of social distancing. Political leaning is the percentage of the state that voted Republican in the 2020 election. The size of the point indicates the number of women of reproductive age in that state during 2020.
Following Wave 1, wave severity was significantly negatively associated with fertility rate change (b = −0.60, 95% CI = −1.19, −0.02); upon covariate adjustment, this association was still negative but attenuated (b = −0.32, 95% CI = −0.69, 0.04) (Table II). For Wave 2, wave severity was not associated with fertility rate change in either simple or multivariable linear regression (Table II). When we additionally controlled for economic impact, the Wave 1 adjusted effect estimate was closer to the null (b = −0.25, 95% CI = −0.58, 0.09) (Supplementary Table SIV). Wave severity was negatively associated with fertility rate change in majority-Democrat states post-Wave 1 (b = −0.83, 95% CI = −1.49, −0.16) and in the same direction but attenuated after covariate adjustment. In majority-Republican states, adjusted Wave 1 results were similar in magnitude but opposite in direction (Supplementary Table SV). For Wave 2, wave severity was not associated with fertility rate change regardless of political leaning (Supplementary Table SVI).
Table II.
Associations between COVID-19 severity and annual change in average monthly fertility rate (births/month/100 000 women of reproductive age/year) in the USA following Wave 1 and Wave 2.
| Predictor | Wave 1 |
Wave 2 |
||
|---|---|---|---|---|
| Unadjusted b (95% CI) | Adjusted b (95% CI) | Unadjusted b (95% CI) | Adjusted b (95% CI) | |
| Wave severity (cases/100 000/month) | −0.60 (−1.19, −0.02) | −0.32 (−0.69, 0.04) | −0.04 (−0.15, 0.07) | 0.01 (−0.11, 0.13) |
| Percentage voted Republican 2020 | 0.45 (0.01, 0.89) | −0.05 (−0.27, 0.17) | ||
| Percentage non-White | −0.90 (−1.25, −0.55) | −0.72 (−0.94, −0.50) | ||
| Affordable housing units | −0.44 (−0.81, −0.07) | −0.34 (−0.57, −0.12) | ||
| Wave timinga | −33.22 (−42.72, −23.72) | −6.66 (−13.17, −0.15) | ||
| R-squared | 0.08 | 0.78 | 0.01 | 0.48 |
Wave 1: Spring versus Summer; Wave 2: Fall versus Winter.
b: beta, effect estimate; COVID-19: coronavirus disease 2019.
Sensitivity analyses
Effect estimates remained virtually unchanged from the original models when we accounted for migration (Supplementary Table SVII). Adjusting for pre-pandemic secular trends in fertility rates did not meaningfully change our regression results for Wave 2 (Supplementary Table SVIII). However, for Wave 1, the effect of COVID-19 wave severity was attenuated (b = −0.14, 95% CI = −0.49, 0.21).
Discussion
In this ecological analysis, we observed a decline in average monthly fertility rate change nationwide 9 months following Wave 1 of the COVID-19 outbreak compared with the already negative pre-COVID secular trend, and a reversal of that decline following Wave 2. These changes varied among US states and across waves resulting in four distinct patterns of annual fertility rate changes from Wave 1 to Wave 2. Analyzing all states together, COVID-19 wave severity was negatively associated with fertility rate change following Wave 1, but not Wave 2. States’ racial/ethnic composition, economic conditions, and political leaning were also associated with post-COVID fertility rate changes. Our results were robust to sensitivity analyses that accounted for population movement and secular trends in fertility decline. Accounting for secular trends, as well as for seasonality of births, which we did by comparing year-over-year fertility rates during the same months, is a vital and overlooked aspect of epidemiological fertility rate studies; failing to do so may lead to spurious results (Gemmill et al., 2022).
Following the 2008 recession, the USA saw an average annual decline of approximately 16 births/month/100 000 WRA/year from 2007 to 2009 (Sutton et al., 2011). Comparatively, we observed an average annual change of −17.5 births/month/100 000 WRA/year following Wave 1, emphasizing the profound impact of COVID-19 on fertility rates in the USA. Nine months after Wave 2, the average annual change was −9.2 births/month/100 000 WRA/year, consistent with the pre-pandemic secular trend. Our national level results align with reported changes in pregnancy intention over a similar period. In a nationwide survey conducted in the first few months of the pandemic, the Guttmacher Institute reported that 40% of US female respondents ages 15–44 years wanted to delay or abandon pregnancy altogether (Lindberg et al., 2020); when they repeated this survey a year later, only 22% of respondents were planning to do so (Lindberg et al., 2021). Similarly, a study conducted in the American Southwest found that, while women aged 15–44 years had less desire to become pregnant when surveyed during the first COVID-19 wave than pre-pandemic, pregnancy intentions were back to pre-pandemic levels when the same participants were surveyed during the second wave (Rocca et al., 2022). Our results are also consistent with international studies: a time-series analysis in 24 European countries found a 14% decline in births 9 months following the first COVID-19 wave, with over half of the countries examined experiencing a birth rate rebound by March 2021 (Pomar et al., 2022).
The rebound we observed in the national fertility rate is consistent with an uptick in births recently reported by the CDC, the first increase since 2014 (Hamilton et al., 2022). While it is possible that this rise is a longer-term shift that will eventually offset the pre-COVID secular decline in the US fertility rate, we suspect that it is more likely a temporary baby boom resulting from pregnancies delayed because of COVID-19 and the fertility rate will soon revert to its pre-pandemic trend. This latter scenario would be in line with reports indicating that a growing number of Americans are choosing to remain childless to satisfy both career ambitions and desires for personal autonomy, and because of concerns about climate change (Cain, 2020; Jenkins, 2020; Brown, 2021).
While our findings conform with previously published reports of national fertility rate declines following the outbreak of the COVID-19 pandemic (Tavernise, 2020; Lewis, 2021), we are the first to investigate if this phenomenon was uniform across the USA and what state-level factors may have contributed to it. There was great variability in fertility rate changes among states in each wave. Pre-COVID, the SD for the annual change in fertility rate was 5.3, whereas it was 23.4 and 8.9 for Wave 1 and Wave 2, respectively. We also observed large variability among states across the two waves. For example, some states, such as New York, experienced large drops in fertility rate followed by only partial recoveries; others, such as Rhode Island, also experienced large drops but rebounded by Wave 2. Meanwhile, Maine showed a large fertility rate increase following Wave 1 that was maintained through Wave 2, while West Virginia showed an initial increase in fertility rate followed by a larger decline. Therefore, while nationally we observed a fertility rate decline following Wave 1 and eventual recovery following Wave 2, this did not occur uniformly across states or in some states at all. Subsequent to our observation of state-level heterogeneity in fertility rate changes during the pandemic, we then tried to identify state-level predictors that might have influenced these changes. While we were underpowered to draw definitive conclusions about how state characteristics influenced fertility patterns across the two waves, we hope that future studies will investigate predictors of these four patterns to better inform our knowledge of drivers of fertility changes in relation to COVID-19 and other crises.
We were curious whether wave severity was associated with state-level annual fertility rate changes. Cohen (2021) previously reported declines in births among nine states in the 9 months after the first COVID-19 wave. In two of these states, county-level infection rates and changes in mobility were significantly associated with birth changes, yet he suggested these results could also be explained by economic, social, and demographic factors, which were unaccounted for in his analysis (Cohen, 2021). In our analysis, expanded to all 50 states and Washington, DC, we only found a significant negative effect of wave severity on fertility rate changes when not adjusted for other state-level factors. Upon stratifying our analysis, it became clear that the effect of wave severity on annual fertility rate changes was driven by majority-Democrat states (majority-Democrat states: −0.38 (−0.89, 0.13) versus majority-Republican states: 0.32 (−0.39, 1.02)). We also observed a slight attenuation of our results following adjustment for the economic impact of the pandemic. One interpretation of this attenuation might be partial mediation by economic impact of the pandemic; however, it might also represent confounding, interaction, or collinearity and requires further investigation with adequately powered data.
Others have suggested that concerns such as unemployment, stress, school closures, social isolation, and general uncertainty about the future could be stronger drivers of changing fertility behavior rather than pandemic severity (Gemmill, 2019; Barroso, 2021). We observed that economic and demographic factors were associated with post-COVID declines in fertility rates in our data. The pandemic has underscored persistent disparities in the USA along racial and economic lines that impact how Americans decide if and when to get pregnant (Stout et al., 2021). Non-White Americans were both more likely to suffer from COVID-19 infection and the economic consequences of the pandemic, largely owing to structural inequalities that impact these groups’ access to health care, financial, educational, and employment resources (Snowden and Graaf, 2021). These groups were also more likely to be disproportionately affected by income loss and food insecurity during the pandemic. Prior studies have shown that economic hardship was a primary predictor of fertility intention during the early months of COVID-19 (Lindberg et al., 2020; Cohen, 2021; Kahn et al., 2021; Lin et al., 2021; Lindberg et al., 2021; Morse, 2021).
While states’ racial composition was significantly associated with fertility rate change in bivariate analysis and included in our regression models, it represents a proxy for a cluster of variables indicating social disadvantage since, in the USA, non-White populations are more likely to live below the poverty line and suffer more financial hardship during periods of economic instability (Lin et al., 2021). Indeed, these sociodemographic variables were largely collinear in our data. The already precarious position of low-income and non-White individuals in US society was likely worsened by the social upheaval caused by the pandemic, potentially resulting in altered pregnancy intentions caused by anxiety about the future. Being low-income and non-White were also important predictors of fertility decline after the 2008 recession (Seltzer, 2019).
Considering that a decline in US fertility rates could impact economic stimulation in light of our increasingly aging population, it has been argued that maintaining a fertility rate near the replacement level is in the national interest (Rogers and Wilder, 2020; Chapman, 2022). Given our findings that state demographic and economic characteristics were associated with fertility decline, the US government could consider adopting policies to alleviate the stressors impacting fertility rates highlighted in this study such as financial strain and social disadvantage. For example, policies that reduce the cost of childrearing, such as paid family leave, may ease obstacles to growing a family, especially in times of crisis (IWPR, 2020). Our research highlights the need for further investigation of how policy interventions might moderate the effect of social vulnerability on fertility rates in the USA.
Strengths and limitations
As an ecological analysis, our study cannot be used to infer individual-level conclusions. It is important to examine influences on fertility on the population level, however, as there may be negative social and economic impacts if the fertility rate falls too steeply (Santacreu, 2016). Another limitation of this analysis is our inability to account for within-state heterogeneity. Studies in Australia and Japan found that local factors, such as urbanicity, are important determinants of both the COVID-19 experience and fertility rates (Ghaznavi et al., 2022; Schoenaker et al., 2022). Data were only available at the state level for this study. We believe future research at the level of counties or other localized geographies are necessary to enrich our findings.
Despite our effort at parsimony, we were still underpowered to detect statistically significant results in covariate-adjusted analyses. We also could not account for how spillover effects from neighboring states or states in the media spotlight might have influenced other states’ responses to the pandemic. Because most pandemic-related economic relief came from the federal government in the form of stimulus cheques, loans, and other help and did not vary by state, we did not account for federal economic relief when conducting analyses pertaining to economic determinants. Nevertheless, our results may still be affected by residual confounding by factors associated with both fertility rates and the pandemic such as ART use, contraceptive access, and potential effects of COVID-19 infection on the ability to conceive and deliver a live birth.
Ours is the first paper to analyze determinants of fertility rate changes since the COVID-19 outbreak using US state-level data for all 50 states and Washington, DC. This contribution to the literature is essential, as the USA is extremely heterogeneous and, as our results demonstrate, varied in its response to the pandemic. We are also the first to analyze fertility rates following the second COVID-19 wave and compare trends to those following the first. We incorporated a wide array of state-level data from a variety of publicly available sources and considered the impact of migration and secular fertility rate decline in sensitivity analyses.
Conclusion
The COVID-19 pandemic exacerbated existing disparities in the USA, including those that influence pregnancy intention and, consequently, fertility rates. We observed a national fertility rate decline following the first wave that amplified the longstanding downward trend in the USA. In addition, we found a remarkable correlation between states’ SDI (which tracked with political leaning) and fertility rate change, suggesting that fertility rate changes as a consequence of the pandemic appear to have been influenced by the level of concern that individuals and state governments placed on mitigating the spread of COVID-19. In sum, our analysis shows that, while fertility rates fell and potentially recovered across the first two COVID-19 waves on a national level, shifts were not uniform across states and largely depended on existing social inequalities and not the severity of the pandemic itself. Building on this ecological study, future epidemiologic investigations should examine individual-level variables that factor into pregnancy decision-making, especially in times of crisis or social change.
Supplementary Material
Contributor Information
Sarah Adelman, Department of Pediatrics, New York University Grossman School of Medicine, New York, NY, USA.
Mia Charifson, Vilcek Institute of Biomedical Graduate Sciences, New York University Grossman School of Medicine, New York, NY, USA; Department of Population Health, New York University Grossman School of Medicine, New York, NY, USA.
Eunsil Seok, Department of Population Health, New York University Grossman School of Medicine, New York, NY, USA.
Shilpi S Mehta-Lee, Department of Obstetrics and Gynecology, New York University Grossman School of Medicine, New York, NY, USA.
Sara G Brubaker, Department of Obstetrics and Gynecology, New York University Grossman School of Medicine, New York, NY, USA.
Mengling Liu, Department of Population Health, New York University Grossman School of Medicine, New York, NY, USA.
Linda G Kahn, Department of Pediatrics, New York University Grossman School of Medicine, New York, NY, USA; Department of Population Health, New York University Grossman School of Medicine, New York, NY, USA.
Data availability
The data underlying this article will be shared upon reasonable request to the corresponding author.
Authors’ roles
S.A.: conception, design, acquisition, analysis, interpretation, drafting, editing. M.C.: conception, design, acquisition, analysis, interpretation, drafting, editing. E.S.: conception, design, analysis, interpretation, editing. S.S.M.-L.: conception, interpretation, editing. S.G.B.: interpretation, editing. M.L.: conception, design, analysis, interpretation, editing. L.G.K.: conception, design, interpretation, drafting, editing.
Funding
L.G.K. received funding from the National Institute of Environmental Health Sciences (R00ES030403), M.C. from the National Science Foundation Graduate Research Fellowship Program (20-A0-00-1005789), and S.S.M.-L. and E.S. from the National Institute of Environmental Health Sciences (R01ES032808).
Conflict of interest
None to declare.
References
- Adolph C, Amano K, Bang-Jensen B, Fullman N, Magistro B, Reinke G, Wilkerson J.. Governor partisanship explains the adoption of statewide mask mandates in response to COVID-19. State Polit Policy Q 2022;22:24–49. [Google Scholar]
- Aitken RJ. The changing tide of human fertility. Hum Reprod 2022;37:629–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey MJ, Bart L, Lang VW.. The missing baby bust: the consequences of the COVID-19 pandemic for contraceptive use, pregnancy, and childbirth among low-income women. Popul Res Policy Rev 2022;41:1549–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barroso A. With a Potential ‘Baby Bust’ on the Horizon, Key Facts about Fertility in the U.S. before the Pandemic Birth Rate & Fertility. Washington, DC.: Pew Research Center, 2021. [Google Scholar]
- Brown A. Growing Share of Childless Adults in U.S. Don’t Expect to Ever Have Children Parenthood. Washington, DC.: Pew Research Center, 2021. [Google Scholar]
- Buckles K, Hungerman D, Lugauer S.. Is fertility a leading economic indicator? Econ J 2020;131:541–565. [Google Scholar]
- Cain S. Why a generation is choosing to be child-free. The Guardian. 2020.
- Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC, 2023. https://covid.cdc.gov/covid-data-tracker.
- Chapman J. The Long-Term Decline in Fertility—And What It Means for State Budgets. Washington, DC.: Pew Trusts, 2022. [Google Scholar]
- Clark WA. Do women delay family formation in expensive housing markets? Demogr Res 2012;27:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen PN. Baby Bust: Falling Fertility in US Counties Is Associated with COVID-19 Prevalence and Mobility Reductions. 2021. https://osf.io/preprints/socarxiv/qwxz3.
- Colleran H, Snopkowski K.. Variation in wealth and educational drivers of fertility decline across 45 countries. Popul Ecol 2018;60:155–169. [Google Scholar]
- De Geyter C. Live birth numbers undulate as crises come and go. Hum Reprod 2022;37:2728–2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Geyter C, Masciocchi M, Gobrecht-Keller U.. Excess mortality caused by the COVID-19 pandemic negatively impacts birth numbers in European countries. Hum Reprod 2022;37:822–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn A. Only 24% of Trump Supporters View the Coronavirus Outbreak as a ‘Very Important’ Voting Issue COVID-19. Washington, DC.: Pew Research Center, 2020. [Google Scholar]
- Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, Nahabedian J, Anderson K, Gilboa SM.. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–June 7, 2020. MMWR Morb Mortal Wkly Rep 2020;69:769–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erwin PC, Mucheck KW, Brownson RC.. Different responses to COVID-19 in four US states: Washington, New York, Missouri, and Alabama. Am J Public Health 2021;111:647–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foundation KF. Status of state medicaid expansion decisions: interactive map. Medicaid. KFF, 2022. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/.
- Gemmill A. Demographic Drivers of the Post-Recessionary Fertility Decline and the Future of US Fertility. New York, NY: Peter G Peterson Foundation, 2019. [Google Scholar]
- Gemmill A, Casey JA, Margerison CE, Zeitlin J, Catalano R, Bruckner TA.. Patterned outcomes, unpatterned counterfactuals, and spurious results: perinatal health outcomes following COVID-19. Am J Epidemiol 2022;191:1837–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaznavi C, Kawashima T, Tanoue Y, Yoneoka D, Makiyama K, Sakamoto H, Ueda P, Eguchi A, Nomura S.. Changes in marriage, divorce and births during the COVID-19 pandemic in Japan. BMJ Glob Health 2022;7:e007866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T, Angrist N, Hale AJ, Kira B, Majumdar S, Petherick A, Phillips T, Sridhar D, Thompson RN, Webster S. et al. Government responses and COVID-19 deaths: global evidence across multiple pandemic waves. PLoS One 2021;16:e0253116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton B, Martin J, Osterman M.. Births: Provisional Data for 2021 Vital Statistics Rapid Release. Hyattsville, MD: National Center for Health Statistics, 2022. [Google Scholar]
- Hellstrand J, Nisén J, Myrskylä M.. All-time low period fertility in Finland: demographic drivers, tempo effects, and cohort implications. Popul Stud (Camb) 2020;74:315–329. [DOI] [PubMed] [Google Scholar]
- IWPR. Paid Family Leave Increases Mothers’ Labor Market Attachment. Washington, DC.: Institue for Women’s Policy Research, 2020. [Google Scholar]
- Jenkins LM. 1 in 4 childless adults say climate change has factored into their reproductive decisions. Morning Consult. 2020.
- Jha A. One virus, two Americas. Foreign Affairs. 2020.
- Kahn LG, Trasande L, Liu M, Mehta-Lee SS, Brubaker SG, Jacobson MH.. Factors associated with changes in pregnancy intention among women who were mothers of young children in New York City following the COVID-19 outbreak. JAMA Netw Open 2021;4:e2124273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearney MS, Levine PB, Pardue L.. The puzzle of falling US birth rates since the great recession. J Econ Perspect 2022;36:151–176. [Google Scholar]
- Koenig LR, Smith Hughes C, Gemmill A, Diamond-Smith N.. Unequal impacts of the COVID-19 pandemic on women's fertility preferences: Evidence from a longitudinal cohort in the United States. SSM Popul Health 2022;20:101305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis T. The pandemic caused a baby bust, not a boom. Scientific American. 2021.
- Lin TK, Law R, Beaman J, Foster DG.. The impact of the COVID-19 pandemic on economic security and pregnancy intentions among people at risk of pregnancy. Contraception 2021;103:380–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindberg L, Mueller J, Kirstein M, VandeVusse A.. The Continuing Impacts of the COVID-19 Pandemic in the United States: Findings from the 2021 Guttmacher Survey of Reproductive Health Experiences. New York: Guttmacher Institute, 2021. [Google Scholar]
- Lindberg L, VandeVusse A, Mueller J, Kirstein M.. Early Impacts of the COVID-19 Pandemic: Findings from the 2020 Guttmacher Survey of Reproductive Health Experiences. New York: Guttmacher Institute, 2020. [Google Scholar]
- Marazzi M. State economic monitor. Total Employment. Washington, DC.: Urban Institute, 2022.
- Marcén M, Molina JA, Morales M.. The effect of culture on the fertility decisions of immigrant women in the United States. Econ Model 2018;70:15–28. [Google Scholar]
- McLaren RA, Trejo FE, Blitz MJ, Bianco A, Limaye M, Brustman L, Bernstein PS, Roman AS, Stone J, Minkoff H.. COVID-related “lockdowns” and birth rates in New York. Am J Obstet Gynecol MFM 2021;3:100476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse A. Fewer babies born in December and January but number started to rise in March. US Births Declined During the Pandemic. United States Census Bureau, 2021.
- Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin-Neelon SE. Associations between governor political affiliation and COVID-19 cases, deaths, and testing in the United States. Am J Prev Med2021;61:115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomar L, Favre G, de Labrusse C, Contier A, Boulvain M, Baud D.. Impact of the first wave of the COVID-19 pandemic on birth rates in Europe: a time series analysis in 24 countries. Hum Reprod 2022;37:2921–2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing, 2022. [Google Scholar]
- Rocca CH, Parra M, Muñoz I, Foster DG, Boscardin WJ, Ralph LJ.. Comparison of pregnancy preferences preceding vs year 1 of the COVID-19 pandemic. JAMA Netw Open 2022;5:e2220093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez CG, Gadarian SK, Goodman SW, Pepinsky TB.. Morbid polarization: Exposure to COVID-19 and partisan disagreement about pandemic response. Polit Psychol 2022;43:1169–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers L, Wilder K. Shift in Working-Age Population Relative to Older and Younger Americans. Washington, DC.: US Census Bureau, 2020. [Google Scholar]
- Santacreu AM. Long-run economic effects of changes in the age dependency ratio. Econ Synop 2016;17. 10.20955/es.2016.17. [DOI] [Google Scholar]
- Schneider D. The great recession, fertility, and uncertainty: evidence from the United States. Fam Relat 2015;77:1144–1156. [Google Scholar]
- Schoenaker D, Bennett C, Grieger JA, Harrison CL, Hill B, Enticott J, Moran LJ, Teede HJ, O'Reilly SL, Lim S.. Association between pregnancy intention and psychological distress among women exposed to different levels of restrictions during the COVID-19 pandemic in Australia. PLoS One 2022;17:e0273339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer N. Beyond the great recession: labor market polarization and ongoing fertility decline in the United States. Demography 2019;56:1463–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden LR, Graaf G.. COVID-19, social determinants past, present, and future, and African Americans' Health. J Racial Ethn Health Disparities 2021;8:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobotka T, Skirbekk V, Philipov D.. Economic recession and fertility in the developed world. Popul Dev Rev 2011;37:267–306. [DOI] [PubMed] [Google Scholar]
- Stout MJ, Van De Ven CJM, Parekh VI, Pardo JL, Garifullin M, Xu M, Fenner DE, Smith RD.. Use of electronic medical records to estimate changes in pregnancy and birth rates during the COVID-19 pandemic. JAMA Netw Open 2021;4:e2111621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton P, Hamilton BE, Mathews TJ.. Recent Decline in Births in the United States, 2007–2009. Hyattsville, MD: National Center for Health Statistics, 2011. [Google Scholar]
- Sweeney MM, Raley RK.. Race, ethnicity, and the changing context of childbearing in the United States. Annu Rev Sociol 2014;40:539–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavernise S. The U.S. birthrate has dropped again. The pandemic may be accelerating the decline. New York Times. New York, 2020.
- University of Virginia Weldon Cooper Center DRG. National Population Projections. Virgnia: UVA, 2018.
- U.S. Census Bureau. Educational Attainment in the United States: 2021. 2022. https://www.census.gov/topics/education/educational-attainment/data.html.
- Zhang SX, Arroyo Marioli F, Gao R, Wang S.. A second wave? What do people mean by COVID waves?—a working definition of epidemic waves. Risk Manag Healthc Policy 2021;14:3775–3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Ghader S, Pack ML, Xiong C, Darzi A, Yang M, Sun Q, Kabiri A, Hu S.. University of Maryland COVID-19 Impact Analysis Platform. College Park, USA: University of Maryland, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared upon reasonable request to the corresponding author.