Abstract
Transcutaneous electrical stimulation is applied in a range of biomedical applications including Transcranial Direct Current Stimulation (tDCS). tDCS is a non-invasive procedure where a weak direct current (<2 mA) is applied across the scalp to modulate brain function. High-Definition tDCS (HD-tDCS) is a technique used to increase the spatial focality of tDCS by passing current across the scalp using <12 mm diameter electrodes.
The purpose of this study was to design and optimize “high-definition” electrode-gel parameters for electrode durability, skin safety, and subjective pain. Anode and cathode electrode potential, temperature, pH, and subjective sensation over time were assessed during application of 2 mA direct current, for up to 22 minutes on agar gel or subject forearms. A selection of 5 types of solid-conductors (Ag pellet, Ag/AgCl pellet, Rubber pellet, Ag/AgCl ring, and Ag/AgCl disc) and 7 conductive gels (Signa, Spectra, Tensive, Redux, BioGel, Lectron, and CCNY-4) were investigated.
The Ag/AgCl ring in combination with CCNY-4 gel resulted in the most favorable outcomes. Under anode stimulations, electrode potential and temperature rises were generally observed in all electrode-gel combinations except for Ag/AgCl ring and disc electrodes. pH remained constant for all solid-conductors except for both Ag and Rubber pellet electrodes with Signa and CCNY-4 gels. Sensation ratings were independent of stimulation polarity. Ag/AgCl ring electrodes were found to be the most comfortable followed by Ag, Rubber, and Ag/AgCl pellet electrodes across all gels.
Keywords: HD-tDCS, tDCS, DC stimulation, skin safety, electrode potential, temperature, pH, subjective pain, electrode, conductive gel
Introduction
The goal of this study was to develop reduced contact area electrode configurations for safe and innocuous DC stimulation across the skin for biomedical applications including enhanced drug delivery (Prausnitz et al., 1993) and electrotherapy. We especially considered the electrotherapy application, transcranial Direct Current Stimulation (tDCS) which involves the passage of a constant direct current (generally 260 μA – 2 mA) through the brain. The spatial focality (targeting) of DC stimulation is considered pivotal for efficacy and safety in many biomedical applications, including tDCS. Focality is limited, in part, by the electrode size used. Traditional tDCS designs include sponge based electrodes, saturated with water, saline, electrode paste, and/or gel (e.g. fatty electrode gels) connected to the stimulator via conductive rubber mesh electrodes, rubber bands, or standard alligator clips. Decreasing electrode-skin contact area can improve spatial focality; however, for a given electrode current, the current density at the skin surface concomitantly increases (Nitsche et al., 2007; Datta et al., 2008; Miranda et al., 2008). Further incentives to reduce electrode size include device compactness, portability, and a potentially increased overall safety profile.
All applications involving transdermal DC stimulation share common safety concerns related to skin irritation. However, distinct safety concerns related to actions on deeper tissue also exist. For example, from the perspective of tDCS safety, it is important to independently consider: 1) pruritic, painful, or injurious effects of electrical currents on the skin (Ledger, 1992; Prausnitz, 1996; Dundas et al., 2007) and 2) potential injurious effects of electrical currents on the brain (Agnew and McCreery, 1987; Merrill et al., 2005; Nitsche et al., 2005; Gilad, 2007; Poreisz et al., 2007; Miranda et al., 2008; Liebetanz et al., 2009; Roth, 2009). The relationship between effects on the skin and any effects on the brain are complex, independent of the electrode montage; from an electrode design perspective these effects should be considered independent of one another (Datta et al., 2009a). Stimulation causing changes at the skin may not have any effect on brain function, and vice versa (Swartz, 1989; Bikson et al., 2009a; Liebetanz et al., 2009). The focus of this study is the optimization of electrode parameters to minimize skin irritation and pain, with a specific goal to engineer small (<12 mm) surface electrode configurations for focal stimulation with DC currents. Such DC stimulation electrodes may be ultimately integrated into stimulation arrays, analogous to high-definition EEG, and are thus termed here “high-definition” DC stimulation electrodes (Datta et al., 2009a,b).
Chemical and physical conditions at the electrode solid conductor site may indicate potential skin hazards during DC stimulation; temperature, pH, voltage, and resistance serve as global measures of the changes occurring at the electrode. For wet surface electrodes, three main “phases” (solid conductor, gel, skin) and thus two interfaces (solid-gel, gel-skin) are considered. Within each material and across each interface, chemical (oxidation/reduction) and/or physical (e.g. heating) processes may occur (Merrill et al., 2003). In addition, through conduction and diffusion, changes in one region may affect another. In designing electrodes, the key solid conductor parameters include its materials, size and shape; gel parameters include chemical composition, shape, and volume (e.g. as determined by the design of a holder).
Several previous studies have considered the safety and comfort level of transcutaneous DC electrical stimulation using specific stimulation protocols (durations, intensities…) and electrode configurations, including metal directly on skin (Molitor and Fernandez, 1939; Prausnitz, 1996; Dundas et al., 2007). The safety and comfort level of “conventional” tDCS which employ large sponge electrodes have also been considered (Prausnitz, 1996; Nitsche et al., 2003; Dundas et al., 2007). In this paper, smaller “high-definition” gel based electrodes suitable for high-definition transdermal DC stimulation were evaluated (Datta et al., 2009a,b). Since temperature, acid/base, and other chemical burns have been suggested to account for DC irritation/damage (Prausnitz, 1996; Merrill et al., 2005), changes in temperature, pH, as well as electrode over-potential (measured on agar gel) and self-reported sensation levels over time were examined. Initial electrode potential experiments screened seven gels (Signa, Spectra, Tensive, Redux, BioGel, Lectron, and CCNY-4) and five solid conductors (Ag pellet, Ag/AgCl pellet, Rubber pellet, Ag/AgCl ring, and Ag/AgCl disc). A subset of gels (Signa, Lectron, CCNY-4); and solid-conductors (Ag pellet, Ag/AgCl sintered pellet, conductive Rubber pellet, and Ag/AgCl sintered ring) were selected for additional tests including subject sensation experiments. Here, we describe how 2 mA of direct current may be applied for up to 22 minutes with minimal skin irritation and discomfort using appropriately designed 12 mm diameter Ag/AgCl ring electrodes and CCNY-4 gel. The safety and advantages of high-definition DC transdermal stimulation is discussed in broader context.
Methods
Electrode configurations: materials and geometry
Five types of solid-conductors were tested in this study: 1) “Ag pellet” (2117 - Silver Wire; Surepure Chemetals, Florham Park, NJ, USA); 2)“Ag/AgCl sintered pellet” (550015-pellet electrode; A-M systems Inc, Carlsborg, WA, USA); 3) “Rubber pellet” (116A-GSR-5, rubber electrode; Austin Medical equipment, Westchester, TX, USA; all pellets were 2 mm(D) × 4 mm(L) resulting in ~ 28 ± 2.5 mm2 solid-conductor-gel contact area); 4) “Ag/AgCl sintered ring” (EL-TP-RNG Sintered; Stens Biofeedback Inc, San Rafael, CA; with outer and inner periphery diameter as 12 mm and 6 mm respectively, resulting in a ~ 140 ± 5 mm2 (taking side surfaces into account) solid-conductor-gel contact area); and 5) “Ag/AgCl sintered disc” (550025, Disc Electrode A-M Systems; with 8 mm diameter resulting in ~ 85 ± 5 mm2 electrode-gel contact area). Each electrode-gel configuration was independently evaluated as an anode or cathode. Plastic holders for all electrodes were used to position electrodes over the skin and standardize gel volume used (Figure 1, bottom row). Plastic holders for all pellet electrodes held ~90 ± 5 mm3 of gel volume with a gel-skin contact area of ~25 ± 2.5 mm2. Customized CCNY-B holders for ring/disc electrodes contained ~280 ± 10 mm3 of gel and provided ~95 ± 5 mm2 gel-skin contact area.
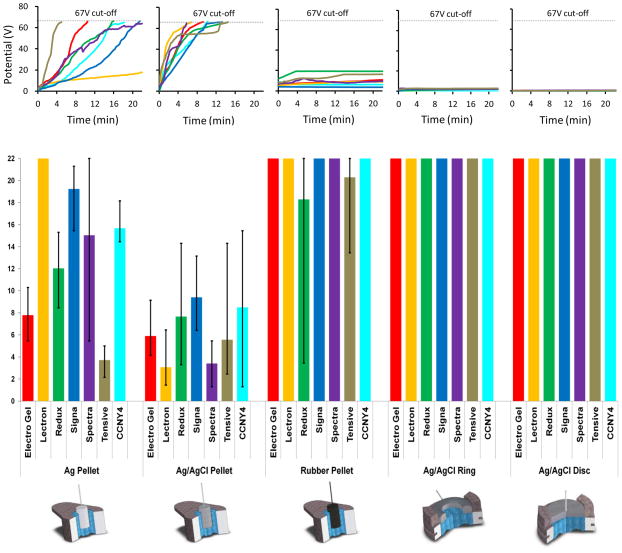
Figure 1.
Average potential and run time profiles during anodal stimulation for the different solid conductor-gel combinations tested.
The following gels were tested: 1) “Signa” (Parker Laboratories Inc., Fairfield, NJ, USA), 2) “Spectra” (Spectra 360, Parker Laboratories Inc.), 3) “Tensive” (Parker Laboratories Inc.), 4) “Redux” (Parker Laboratories Inc.), 5) “BioGel” (1090 BioGel, UFI Inc., Morro Bay, CA, USA), 6) “Lectron” (Lectron II, Pharmaceutical Innovations Inc., Newark, NJ, USA), and 7) “CCNY-4” (custom made). Gels were selected to represent a range of electrical and thermal conductivities. All gels were at room temperature at the time of application. The electrical conductivity values of the gels, measured by a conductivity meter (Model 2052; VWR International LLC, Bridgeport, NJ, USA), were (in units of S/m): CCNY4 ~ (4.5 ± 1.0), Signa ~ (4.0 ± 1.0), Redux ~ (3.5 ± 1.0), Lectron ~ (1.5 ± 7.5), BioGel ~ (1.5 ± 7.5), Tensive ~ (6.0 ± 3.0), and Spectra ~ (1.5 ± 5.0). The thermal conductivity values of the gels, measured by a thermal properties meter (Model KD2; Decagon, Pullman Washington, USA), were (in units of W/m°C): CCNY4 ~ (0.0326 ± 0.0043), Signa ~ (0.0285 ± 0.0034), Redux ~ (0.0326 ± 0.0043), Lectron ~ (0.0285 ± 0.0008), BioGel ~ (0.0280 ± 0.0008), Tensive ~ (0.0295 ± 0.0024), and Spectra ~ (0.0274 ± 0.0007).
DC Stimulation and Resistance
A constant current stimulator (CX 6650, Schneider Electronics, Gleichen, Germany) was used to apply direct current for all trials, with a maximum driving voltage capability of 66.7 Volts. A current intensity of 2 mA was used for up to 22 minutes, with automatic on and off ramps of 10 sec to avoid “stimulation break” effects. The stimulator automatically terminates stimulation at an output potential (total potential across both electrodes and agar/tissue) of 66.7 V (electrochemical reactions may increase electrode potential; see discussion), which was used as a cut-off point in all trials. Prior to and after stimulation, total cell resistance (see below) of the agar gel or forearm skin was measured using a RMS digital multimeter (FLUKE 177; FLUKE Corporation, Everett, WA, USA).; stimulation was only initiated when the total cell resistance was less than 8 MΩ.
Electrode Potential, pH, and Temperature Studies
For studies measuring electrode potential (total potential over the entire assembly of electrodes, gel, and skin), pH, and temperature changes, the electrodes were mounted with gel on a flat block of agar (pH of 6.0) made with 150 mM (physiological) NaCl (Tallgren et al., 2004). Electrode potential experiments were conducted on seven gels (Signa, Spectra, Tensive, Redux, BioGel, Lectron, and CCNY-4) and five solid conductors (Ag pellet, Ag/AgCl pellet, Rubber pellet, Ag/AgCl ring, and Ag/AgCl disc). For these studies, the rationale was to measure changes at only one “active” anode or cathode electrode without contribution from the two “return” electrodes (generally sintered Ag/AgCl disc (84 ± 5 mm2) or ring electrodes (140 ± 5 mm2), each immersed in an excess of ~400 ± 10 mm3 Signa). Based on the electrode potential experiments (see below) we were able to confirm a negligible potential contribution from the two return electrodes. The total cell resistance reflected the resistance between the active electrode and the two return electrodes which were connected in parallel.
For electrode potential experiments, 2 mA DC current was passed through agar gel between an active and return electrode, with an additional passive “reference” electrode (an 8 mm sintered Ag/AgCl disc electrode immersed in Signa gel of volume in excess of ~ 400 ± 10 mm3) placed away from the current path. Changes in electrode potential were simultaneously recorded between the active and return electrode as well as the active and reference electrode. It is expected that the only voltage that will change substantially as a result of stimulation is the voltage across the active electrode. Thus, the electrode potential measurements in these experiments largely reflect the voltage drop at the active electrode (Merrill et al., 2003). The total cell potential is then a summation of the voltage drop across the active and return electrode, and agar gel.
For pH, temperature, and sensation studies, 2 mA of DC current was applied for up to 22 minutes between either an “active” anode or cathode electrode, and two parallel “return” electrodes. The electrodes were placed in a linear conformation with the active electrode placed in the center and two return electrodes, (one on each side of the active electrode) each positioned 5 cm from the active electrode. The use of the two large return electrodes (immersed in excess gel) is intended to minimize total cell potential, chemical reaction, and sensation at return sites.
A micro pH electrode (Orion 9810BN; Thermo Scientific, Waltham, MA, USA) and a pH meter (SM100; Milwaukee Instruments Inc., Rocky Mount, NC, U.S.A.) were used to measure pH in the active electrode’s gel at the agar surface at various exposure durations. To measure the pH, the stimulation was turned off, the solid conductor was removed from the gel, and the micro pH electrode was inserted into the gel within 5 seconds. pH was recorded after exposure durations of 1 min, 5 min, 10 min, 15 min and 20 min. pH studies were conducted on four solid-conductors (Ag pellet, Ag/AgCl sintered pellet, Rubber pellet, Ag/AgCl sintered ring) in combination with three electrolyte gels (Signa, Lectron, CCNY4). For temperature experiments, a Type T Thermocouple Thermometer (BAT–10; Physitemp Instruments, Clifton, NJ, USA) was used on the bottom surface of the agar gel during stimulation.
As indicated above, the stimulator automatically stopped stimulation if a total potential of 66.7 V (cut-off voltage) was achieved. In cases when stimulation was applied for 22 minutes, the “stimulation time” was scored as 22 minutes and the maximum pH and temperature changes during the 22 minutes were noted. In cases when a potential of 66.7 V was reached prior to 22 minutes, the “stimulation time” was scored as the time when the potential reached 66.7 V; the maximum pH and temperature at this “stimulation time” was then noted
Subjective Sensation
Eight healthy subjects (6 males and 2 females; 19–35 years) participated in the study. All gave written informed consent before being included in the study. The study was approved by the IRB board of the City College of New York. Sensation tests were restricted to four solid-conductors (Ag pellet, Ag/AgCl sintered pellet, Rubber pellet, Ag/AgCl sintered ring) and three gels (Signa, Lectron, and CCNY4). For sensation studies, the rational was to determine the effect of the “active” anode or cathode electrode. Two Ag/AgCl ring electrodes were used as “return” electrodes. Return electrodes were positioned on opposite sides of the active electrode. Each return electrode was immersed in excess of ~ 400 ± 10 mm3 volume of Signa Gel. The experiments were conducted on the distal or proximal forearm, as arbitrarily preferred by the subjects. There were no steps taken to otherwise prepare the skin prior to stimulation. Evidently, abrasion effects skin properties. However, these steps were avoided for two reasons: 1) to test the effect of electrical stimulation on unconditioned skin and 2) experimental ambiguity regarding the precise degree of abrasiveness. Regions of skin with visible irritation or cuts prior to stimulation were avoided.
Stimulation was applied for up to 22 minutes with subjects scoring pain (on a 1 to 10 analog scale) every minute beginning two minutes before (t=−2 to t=−1), every minute during (t=0 to t=22), and ending two minutes after stimulation (t=23 to t=24). In addition, subjects were prompted to describe the sensations (“burning”, “prickling” etc.). Prior to stimulation each subject indicated a personal termination value (at or below 5) at which stimulation would be stopped by the operator. In addition, each subject could withdraw from the stimulation at any point of the experiment, regardless of the current pain score or nature of perception. If stimulation was stopped prior to 22 minutes of exposure, the pain rating at termination was noted. Greater than 1 hour of delay was allowed between experiments, and the stimulation site (e.g. arm) was changed for consecutive experiments. Participants were blinded to the type and combination of solid-conductor and gels tested. After stimulation any skin irritation or redness was noted.
Results
Electrode Potential
Electrode potential across conductive agar was recorded during 2 mA DC stimulation. During clinical stimulation it is desirable to minimize electrode potential for several reasons including: 1) voltage limits on constant current stimulators; 2) increased risk for skin injury including through electrochemical reactions (limited by electrode over-potential; the difference between the electrode’s potential and it’s equilibrium potential (both measured with respect to some reference electrode), Merrill et al., 2005) and heating.
Cathodal stimulation with rubber pellets resulted in variable voltage increases whereas electrode potential remained less than 1 V for all other solid-conductors (not shown).
Electrode potential results for anodal stimulation experiments are summarized; we report both the average potential (Figure 1) and variability across trials (Supplementary Figures 1A–E; 5 trials per electrode/gel combination). These potentials can also be interpreted as reflecting changes in the resistance of the electrode during DC anodal stimulation. Using the Ag/AgCl sintered pellets, the full 22 minutes of anodic stimulation could not be applied in combination with any gel. Using the Ag pellet, 22 minutes of anodic stimulation could be consistently applied only with Lectron; after stimulation, a removable, black paste-like residue was observed along the surface of the electrode that could be easily deterged (see discussion). Using the Rubber pellet, significant variability in exposure time was observed across various trials and gels; after stimulation, a relatively thick deposition layer was observed on the rubber. This layer was easily deterged and an apparently intact rubber surface remained. Using both Ag/AgCl sintered ring and Ag/AgCl disk electrodes, 22 minutes of stimulation could be consistently applied, in combination with any gel, with Ag/AgCl disk having the lowest average electrode potentials (Figure 1-e)
Temperature and Gel pH
For pH and temperature measurements we investigated three gels: two with chloride (Signa and CCNY-4) and one nominally chloride free (Lectron); each gel was independently tested in combination with four solid-conductors (Ag pellet, Ag/AgCl sintered pellet, Rubber pellet, Ag/AgCl sintered ring). All measurements were conducted on agar gel (150 mM of NaCl). The baseline pH for all gels was 6.0. Both anodal and cathodal stimulations were tested independently. In the cases where the total cell potential (including electrode potential) exceeded the stimulator cut-off (66.7 V), measurements were limited to the maximum exposure time allowed prior to cut-off.
Cathodal stimulation, which results in minimal electrode potential values did not induce significant temperature increases in the gel under any condition tested (Table 1). For anodal stimulation, in cases where no electrode potential change occurred (e.g. Ag/AgCl sintered ring with any gel) no temperature changes were observed in the gel (Table 1). Across all three tested gels, temperature rises were observed under anodal stimulation with both Ag pellet and Ag/AgCl sintered pellet solid conductors, where electrode potential changes were also maximal. During stimulation with Rubber pellet, there was significant trial-to-trial variability in the temperature changes induced; however, when voltages increases were observed, temperature increased monotonically (though not linearly) with voltage and time. Temperature changes in gel under electrode may thus be avoided by limiting changes in electrode potential. For a fixed electrode configuration (pellet), a change in potential was qualitatively related with a change in temperature.
Table 1.
Summary of cathodal and anodal pH, temperature (on agar gel), and subjective sensation experiments for all eight subjects. The following is summarized: (1) single highest pain score over the duration of stimulation, (2) average pain score for “stimulation time” (see methods), (3) % of subjects that withdrew at any time during the course of the experiment, based on any criteria (see Methods), (4) % of subjects with minor bumps and/or skin blemish evident after stimulation, (5) change in gel temperature (agar gel stimulation), and (6) recorded pH after stimulation (baseline pH of 6.0; agar gel stimulation).
| Anodal | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Electrode | Ag Pellet | Ag/AgCl Pellet | Rubber Pellet | Ag/AgCl Ring | ||||||||
| Gel | Signa | Lectron | CCNY | Signa | Lectron | CCNY | Signa | Lectron | CCNY | Signa | Lectron | CCNY |
| Pain Score High | 3.5 ± 0.7 | 4.5 ± 0.7 | 3.7 ± 0.5 | 3.2 ± 0.9 | 4.5± 0.9 | 3.4 ± 1.9 | 3.6 ± 1.4 | 4.8 ± 1.1 | 3.3 ± 1.5 | 3.0 ± 1.0 | 3.5 ± 0.9 | 3.1 ± 1.2 |
| Pain Score Avg. | 2.5 ± 0.5 | 3.9 ± 1.2 | 2.4 ± 1.0 | 2.4 ± 1.0 | 4.2 ± 1.0 | 2.7 ± 1.6 | 2.9 ± 1.6 | 4.3 ± 1.1 | 2.5 ± 1.5 | 2.0 ± 0.4 | 3.0 ± 1.0 | 2.0 ± 0.9 |
| Withdraw % | 0 | 50 | 0 | 0 | 50 | 20 | 33 | 50 | 20 | 0 | 25 | 0 |
| Skin Blisters | 0 | 16.6 | 0 | 17 | 16.6 | 0 | 16.6 | 16.6 | 20 | 16.6 | 0 | 0 |
| ΔT (°C) | 1.9 ± 1.3 | 1.1 ± 0.8 | 4.1 ± 2.1 | 2.0 ± 1.5 | 3.3 ± 2.8 | 4.5 ± 0.9 | 0.1 ± 0.2 | 0.2 ± 0.2 | 0.05 ± 0.1 | 0.05 ± 0.1 | 0.05 ± 0.1 | 0.05 ± 0.1 |
| pH after stimulation | 5.9± 0.0 | 6.0 ± 0.0 | 5.9 ± 0.0 | 5.9 ± 0.0 | 6.0 ± 0.0 | 5.9 ± 0.0 | 1.5 ± 0.5 | 6.0 ± 0.0 | 1.2 ± 0.7 | 5.9 ± 0.0 | 6.0 ± 0.0 | 5.9 ± 0.0 |
| Cathodal | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Electrode | Ag Pellet | Ag/AgCl Pellet | Rubber Pellet | Ag/AgCl Ring | ||||||||
| Gel | Signa | Lectron | CCNY | Signa | Lectron | CCNY | Signa | Lectron | CCNY | Signa | Lectron | CCNY |
| Pain Score High | 3.4 ± 0.7 | 3.6 ± 0.7 | 4.1 ± 0.5 | 4.4± 0.8 | 4.6± 1.6 | 4.0 ± 1.4 | 4.1 ± 0.5 | 4.3 ± 0.8 | 3.2 ± 1.6 | 3.2 ± 1.6 | 3.8 ± 0.9 | 3.2 ± 1.3 |
| Pain Score Avg. | 2.4 ± 0.5 | 3.3 ± 1.2 | 3.1 ± 1.6 | 3.5 ± 1.6 | 3.7 ± 1.4 | 2.4 ± 1.5 | 3.0 ± 1.3 | 3.7 ± 1.2 | 3.2 ± 1.6 | 1.7 ± 0.7 | 3.0 ± 1.0 | 2.4 ± 1.5 |
| Withdraw % | 0 | 16.6 | 50 | 50 | 50 | 40 | 16.6 | 50 | 40 | 0 | 25 | 20 |
| Skin Blisters | 83 | 67.6 | 0 | 33 | 33 | 20 | 83.3 | 67.6 | 0 | 0 | 75 | 20 |
| ΔT (°C) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| pH after stimulation | 12.5 ± 0.7 | 6.0 ± 0.0 | 13.5 ± 0.4 | 5.9 ± 0.0 | 6.0 ± 0.0 | 5.9 ± 0.0 | 12.5 ± 1.0 | 5.9 ± 0.1 | 12.7 ± 0.7 | 5.9 ± 0.0 | 6.0 ± 0.0 | 5.9 ± 0.0 |
While using Lectron gel, no pH changes were found across all tested electrodes, for either polarity. In the case of Ag/AgCl sintered pellet and Ag/AgCl ring, no pH changes were observed, under either cathodal or anodal stimulation, for all three gels. Using Ag pellet, no pH changes were observed during anodal stimulation, while pH alkalization was observed with Signa and CCNY-4 gel during cathodal stimulation. Rubber pellets, only in combination with Signa and CCNY-4 gel, resulted in acidic gel pH with anodal stimulation and basic gel pH in cathodal stimulation even in the absence of a voltage change. Thus, while increase in temperature is linked to increased electrode potential, pH changes are not clearly linked to electrode potential, and are highly material specific; pH changes can be avoided using appropriate solid-conductor and gel combinations.
Subjective Sensation
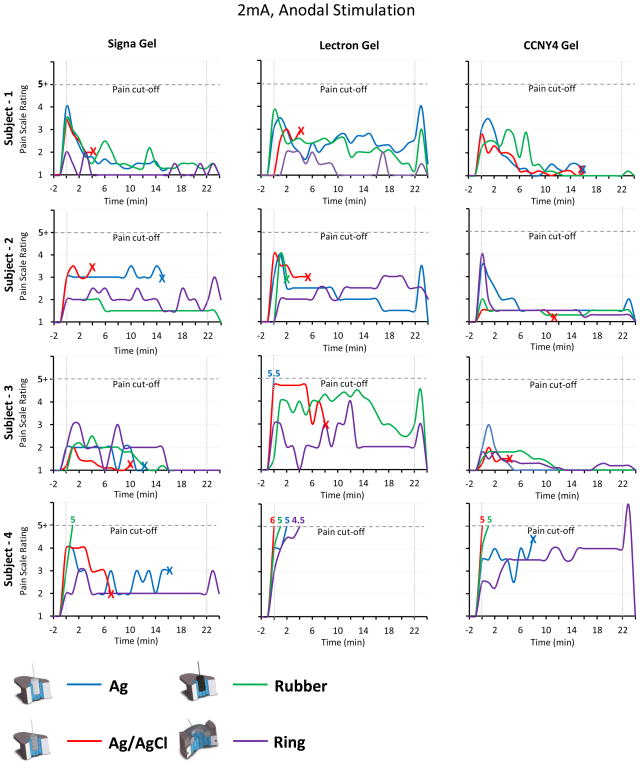
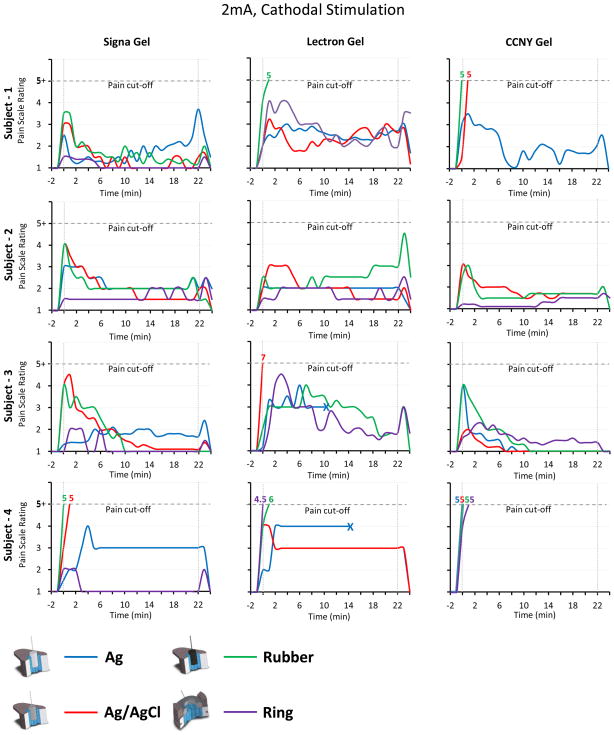
N–way (gel, polarity and electrode) ANOVA was applied to the pain ratings. ANOVA revealed a significant effect of gel (F(1,8) = 10.37, p = .0001) and electrode (F(1,8) = 3.38, p = .019) on pain ratings. There was no effect of polarity (F(1,8) = 0.05, p = .831) or interaction effects of gel-polarity (F(1,8) = 0.72, p = .488), gel-electrode (F(1,8) = 0.33, p = .922), polarity-electrode (F(1,8) = 0.13, p = .944) and gel-electrode-polarity(F(1,8) = 0.37, p = .897). Overall, Signa and CCNY-4 were better tolerated than Lectron. There was no significant difference between anodal verses cathodal stimulation.
The results for all eight subjects are summarized in Table 1. Across subjects, stimulation polarity, electrode gel, and configurations, subjective sensation was highest when stimulation was ramped on or off (Figure 2, Figure 3). As expected for any relative individual pain scoring, there were differences in absolute levels between subjects as well as differences in conditions tolerated (e.g. Figure 2, compare Subject 2 and Subject 4). A majority of subjects indicated that sensation was restricted only to the “active” test electrode (anode or cathode), but in a few cases subjects indicated sensation under the return electrode(s); this was not an exclusion criteria. There was no evident correlation between gel pH or temperature changes (Table 1) to that of the subject sensation; for example Ag/AgCl sintered ring electrodes resulted in no gel temperature or pH changes but did induce discomfort in some subjects.
Figure 2.
Subjective sensation scores of four subjects during 22 minutes of anodal stimulation (t=0 to t=22), for each solid conductor-gel combination. The symbol “X” denotes the termination of stimulation (output potential of 66.7 V has been reached). Four subjects were randomly selected to illustrate the individual time course of scores.
Figure 3.
Subjective sensation scores of four subjects during 22 minutes of cathodal stimulation (t=0 to t=22), for each solid conductor-gel combination. The symbol “X” denotes the termination of stimulation (output potential of 66.7 V has been reached). Four subjects were randomly selected to illustrate the individual time course of scores.
Examination of the skin after stimulation indicated transient redness. Overall, in cathodal stimulations there are higher chances of observing skin irritation in the form of small bumps or black dots (<1 mm) and apparent roughening of the skin under the electrode (Berliner, 1997; Geddes and Roeder, 2004). Observation of bumps or dots was not apparently correlated to subjective pain sensation, polarity, or any physical gel changes (Table 1). All effects on the skin were reversible and disappeared within few hours. No subject reported a lasting irritation or pain.
We observed no consistent relationship between the changes in electrode potential and skin sensation during stimulation (or redness post-stimulation). The average cell resistance prior to stimulation with Ag/AgCl ring electrode ranged from 100 kΩ to 8 MΩ (average 675 ± 1100 kΩ). After the stimulation, the tissue resistance significantly reduced to a range of 3 kΩ to 800 kΩ (average 68 ± 272 kΩ). The average percentage drop of resistance resulting from stimulation was 92% ± 67%.
Discussion
Transcutaneous DC stimulation at increasing current densities
This study was motivated by the need to develop smaller electrodes for transcutaneous DC stimulation; the most common current applications being transdermal drug delivery (Ledger, 1992; Prausnitz, 1996; Dundas et al., 2007) and electrotherapies including transcranial DC stimulation (Prausnitz, 2006; Datta et al., 2009a; Nitsche et al, 2007). The most evident advantage of smaller electrodes is increased therapy focality (as the tissue targeted focality is presumably limited by electrode contact area), but additional advantages may be related to robustness and safety, portability, and the ability to use arrays of electrodes.
There is simultaneously a desire to increase the levels of current to enhance existing transcutaneous DC therapies. The main conceptual limitation in adapting smaller DC stimulation electrodes is the perception that increased electrode current densities will invariably lead to skin irritation and/or injury. The results of this study, though only an initial investigation of selected configurations, indicates that rational optimization of electrode design can facilitate innocuous and safe therapy at increased DC current densities. Conversely, when using non-optimized electrodes, such as tap-water soaked sponges, hazards may increase compared to using smaller but rationally designed electrode; for example poor electrode design can result in current concentration at electrode edges or discontinuities leading to unpredictable hazards (see below).
Still further insight into the mechanism of discomfort and electrode development may rationally reduce residual irritation to negligible levels. In electrode design, it is critical to distinguish between effects at the skin and any other (therapeutic) effects of stimulating deeper tissue (e.g. brain modulation); the two are not necessarily linked and this study only addresses effects at the skin (Bikson et al., 2009a). Equally important to emphasize is that specifics of electrode design are paramount, such that under non-ideal conditions (e.g. metal on skin) even small voltages (e.g. 9 V) can lead to tissue damage (low voltage burns, (Geddes and Roeder, 2004)); for this reason it is not prudent to directly extrapolate hazards from previous studies in which different electrode/gel configurations were used (Prausnitz 1996; Martinsen et al., 2004; McCreery et al., 1990; Dundas et al., 2007). None-the-less, in the following discussion we consider our specific electrode design referencing a broader mechanistic context both to interpret our findings and support further rational electrode design for high-definition transcutaneous DC stimulation.
The solid-conductor, gel, and skin form three distinct phases – with two interfaces. In the solid-conductor and in attached electrical circuits, charge is carried by electrons. In saline gel and tissue – or in more general electrochemical terms, in electrolytes – charge is carried by ions, such as sodium, potassium, and chloride. The central process that occurs at the solid-conductor/electrolyte interface is electrochemical transduction of charge carriers from electrons to ions (reviewed in Merrill et al., 2005). Prolonged DC current, in particular, can drive electrochemical reactions that are hazardous to tissue or degrade the electrode. The composition and dimensions of the solid-conductor/gel interface fundamentally determine the nature of these reactions. The “bulk” gel acts as a barrier (buffer) between this interface and the skin, and may also itself respond to passing current (e.g. gel heating and/or denaturing). Importantly, the ultimate pruritic response reflects only how these reactions influence conditions at the skin, as well as direct response to current flow in the skin; these issues are considered in the next two sections.
Electrochemistry of surface DC stimulation
We propose the following electrochemical scheme: when electrode/gel conditions exist to support AgCl depletion/formation at the cathode/anode, DC electrical stimulation can proceed with minimal over-potential and no pH or temperature change. When AgCl depletion/formation is no longer supported during the course of stimulation, electrode over-potential increases. This then leads to additional chemical reactions, which, in turn, may ultimately lead to heating and pH changes. Over-potentials do not necessarily lead to (or are sufficient for) such changes, but are necessary for additional chemical reactions to occur.
For DC stimulation, a common approach is to use Ag/AgCl non-polarizing electrodes. The rationale for this approach is that, as long as Ag/AgCl formation/depletion can proceed (faradaic charge-transfer reactions; Merrill et al., 2005), no electrode over-potential develops and thus no other electrochemical processes initiate. At the cathode, dissolution of silver chloride and reduction of the silver ions facilitates faradaic charge delivery across the electrode.
| (1) |
At the cathode, AgCl is thus depleted from the electrode surface. Under our tested conditions using all Ag/AgCl electrodes (both pellet and ring), the availability of AgCl was apparently sufficient to allow this cathodic reaction for 22 minutes at 2 mA and hence minimal over-potential was generated; this proceeded independent of gel composition (the baseline concentration of Cl− in the gel being irrelevant, as it is a product). For similar reasons, no pH or temperature changes were observed during cathodal stimulation with any AgCl electrodes, independent of gel composition.
At the anode electrode site AgCl is formed.
| (2) |
In contrast to the above described cathodal process; this anodal process requires Cl− availability in the gel and Ag at the solid-conductor surface. One might then predict that anodal stimulation with Ag pellet and Cl− rich gel (Signa, CCNY-4) would produce the least over-potential and longest run times because reaction (2) is supported. However, results show that high-over potentials developed during anodal stimulation of Ag pellet with Cl− rich gel. Our hypothesis, in this special case, is that due to the rate of reaction (2) there is a rapid formation of AgCl on the metal electrode, which may appear as a black deposition layer on the electrode. This layer may “chemically insulate” the electrode from further reactions, which in turn may explain the increase in the electrode over-potential and decrease in run time. This hypothesis is supported by our observation that after removing this deposition layer, a second stimulation supports run times comparable to the novel case of the Ag pellet electrode, while running a second stimulation without removing the deposition layer results in run times of less than a minute. Conversely, anodal stimulation with Ag pellet in the presence of a nominally Cl− free gel (Lectron) did not produce high over-potentials suggesting that the oxidation of Ag to Ag+ is supported with another (unknown) abundantly present anion (we found no evidence for pH change, rejecting the possibility of significant hydrolysis at the anode during stimulation with Ag pellet (see below)). The failure of Ag/AgCl pellets to support anodic stimulation may indicate 1) the formation of a similar chemical insulation layer; or 2) insufficient reservoir of available Ag.
We used micro-temperature and pH sensors to detect physical/chemical changes in the gels under the electrodes during stimulation. We cannot rule out that during stimulation across skin, hot-spots of temperature or pH changes may occur, for example in sweat glands, which could not be measured in our protocol (see below). At the gel, we observed pH changes only with pellet electrodes and specific solid-conductor/gel combinations. pH changes reflect electrochemical reactions at the solid-conductor/gel interface and the (in)ability of the gel to then buffer pH changes. For example, in the case of cathodal stimulation with Ag and Rubber pellets (where reaction (1) was not supported), significant pH changes were observed only in combination with Signa and CCNY-4 gel. When pH changes were observed, the anode site became more acidic and the cathode site more basic; this observation is consistent with oxidation of water at the anode site (formation of H+) and reduction of water at the cathode site (formation of OH−; reviewed in Merrill et al., 2005);
| (3) |
| (4) |
In all cases where the electrode/gel combination was expected to support AgCl formation (anode) or depletion (cathode), except for Ag/AgCl pellet, pH changes were not observed. This is consistent with the reduction/oxidation of water, which requires higher electrode over-potential to initiate than AgCl formation/depletion. However, in cases where the respective AgCl reaction was not supported, changes in pH were not necessarily observed, reinforcing the importance of the specific electrode-gel design. Our observation of acidification at the anode and alkalization at the cathode is consistent with previous pH measurements using various types of electrodes (Ledger et al., 1992; Cooper et al., 1996; Geddes and Roeder, 2004; Merrill et al., 2005).
We should note that a range of additional reactions can occur at the solid-conductor/gel interface, as the electrode potential increases for example corrosion and Cl2 gas formation at the anode (Leeming et al., 1970; Cooper et al., 1990; Merrill et al, 2005). Whereas corrosion or formation of gases (e.g. hydrogen, oxygen, and chloride gas) may be catastrophic for (chronic) implanted electrodes, these reactions are not necessarily injurious for skin surface (replaceable) electrodes. Therefore, as reinforced throughout this discussion, safety studies using implanted electrodes (generally with distinct materials, configurations, and absence of gel) cannot simply be used to determine quantitative guidelines for non-invasive stimulation.
Conductive Rubber electrodes cannot support either AgCl depletion at the cathode (1) or AgCl formation at the anode (2). The chemical reactions occurring at the rubber-gel interface are poorly defined, and though they may support prolonged stimulation, there was trial-to-trial variability in induced potential and associated temperature and pH changes. Pilot experiments on skin sensation also indicated trial-to-trial variability using Rubber electrodes; moreover, during the course of stimulation, unpredictable spikes in pain were observed.
Temperature increases can result from electrically driven chemical reactions at the electrode/gel interface and joule heating as current flows across the gel. We could not establish a simple relationship between electrode potential and temperature, but results show that a lack of voltage change indicated no significant gel temperature rise. A persistent (i.e. long duration) macroscopic (e.g. water bath) temperature rise of 45°C is cited as a safety limit for skin burns (Peters and Rossiter 1992, Cranne-van Hinsberg et al., 1995; Prausnitz 1996) and references therein p408) which was not achieved under any conditions tested here.
No pH changes were observed using ring shaped electrodes in combination with any gel. A simple explanation for this is that for the 2 mA <22 minutes exposure tested here, the increase in solid-conductor/gel contact area when moving from pellet to ring shapes, results in a critical increased capacity for charge transfer (for the case of AgCl). Because no over-potentials resulted from stimulation with the Ag/AgCl sintered ring electrode, no significant changes in pH or temperature changes in the gel were observed.
Skin response to DC stimulation, Mechanisms of skin irritation and pain
Skin responses to DC electrical stimulation have been previously studied – electrode design is paramount to both the qualitative and quantitative nature of effects. As summarized above, using our electrode designs, limiting electrode potential is an effective method to prevent significant temperature and pH changes, however, for some subjects, sensation was reported in the absence of a voltage change. Thus voltage and polarity could not be used to simply predict the pain sensation or skin irritations, and pain could not be consistently correlated with gel pH or temperature changes. Though gel pH and temperature are considered indicative of a potential hazard (though we could not establish here a clear causative relationship), from the perspective of clinical application, prevention of pain and skin irritation is the most relevant outcome. The chemically (pH) and temperature-wise inactive Ag/AgCl ring electrode still resulted in significant skin sensation in some subjects. There was significant variability across subjects, which could not be predicted based on the physical parameters we measured. Peak sensation was correlated with stimulation being ramped on and off; the “habituation” to on stimulation has been reported elsewhere (Prausnitz, 1996). The period of maximum sensation (when the current was ramped on and off) is not apparently linked to maximum pH and temperature changes at any gel.
In the absence of gel pH or temperature change, we can only speculate about the causes of sensation during stimulation with Ag/AgCl sintered ring electrode. One explanation is that (lack of) ‘bulk’ pH or temperature change in the gel does not reflect changes in the skin, including across skin layers (Molitor and Fernandez, 1939; Martin et al., 2002; Pliquett et al., 2002, Datta et al., 2009b). Moreover, skin inhomogeneities, such as sweat glands or pre-existing lesions, may form conductive pores that funnel current leading to microscopic “hot spots” of chemical or temperature changes within the skin (Mason and Mackay, 1976; Wiley and Webster, 1982; Ledger, 1992; Panescu et al., 1994; Prausnitz, 1996; Pliquett et al., 2002) or across skin layers (Prausnitz, 1996). Chemical or temperature changes could then lead to changes in neuronal activity and sensation/pain. Under their experimental conditions, Yoshida and Patriciu, 2003, correlated localized current concentrations with pH changes and burns. The “hot spot” hypothesis may account, in part, for habituation to pain, as DC stimulation “homogenizes” skin properties (see below) but not evidently for increased sensation when stimulation is turned off. This hypothesis is also consistent with (though not proven by) our observation of small red or black spots, often localized at hair follicles, after DC stimulation (as has been observed by others; references (Mason and Mackay, 1976; Ledger, 1992)); though we could not simply correlate the observation of spots with sensation/pain during stimulation. In a few subjects, subjective skin perception lasted several minutes after the current was switched off; assuming this reflects a true peripheral action, nerve excitation due to pH/temperature change in the skin may be one of the reasons of pain persistence (Martinsen et al., 2004).
In addition, to microscopic pH/temperature changes within the skin (above), the most parsimonious explanation for irritation is electrical activation of nerve fibers. Indeed, the basis for electrotherapy is the modulation of nervous system function by electricity (Bikson et al., 2009b). The theory of electrical stimulation has been extensively studied (Merrill et al., 2005). The “accommodation” of axonal responses to DC stimulation could account for the sensation habituation after stimulation is turned on (Kiernan et al. 2002), while anodic break type phenomena could explain sensation as stimulation is turned off.
DC stimulation across the skin can increase local blood flow (Ledger, 1992; Prausnitz, 1996; Berliner 1997; Malty and Petrofsky, 2007) leading to erythema (“redness” resulting from presumed capillary dilation) under the electrodes – this is not in itself hazardous and in fact has been used for therapeutic purposes (e.g. “hydrogalvanic baths”, drug delivery). Cause of vasodilatation can include pH changes (both acidosis and alkalization) in the skin, secondary actions to nerve or smooth muscle activation, and/or a range of biological responses, such as release of neuropeptides in response to electric fields (Ledger et al., 1992; Berliner, 1997). Temperature changes will both effect and be modulated by changes in blood flow. Dilation may itself be heterogeneous (“hot spots”) under certain conditions (Berliner, 1997; Droog and Sjoberg, 2003). In this study, we could not correlate erythema with pain, nor is there an evident mechanistic link between erythema and either an analgesic or pruritic effect. Berliner (1997) reports increased erythema (and moderately increased temperatures) under cathodal stimulation compared to anodal, but no subjective perceived differences. Alternatively, an analgesic effect has been proposed. Unrelated skin injury can lead to an inflammatory response. Large current can damage blood vessels (Rouge et al. 1994) but not at the intensities used in the present study. In summary both the causes of erythema and its impact on paresthesia remain unclear, yet the ubiquity of this phenomena under a broad range of stimulation conditions, indicates it merits further investigation.
It is well established that transdermal stimulation changes skin properties including increasing skin conductivity and porosity (Prausnitz 1996; Prausnitz et al. 1993); this has been termed “electro-osmosis” or “electroporation”, though the specific mechanisms remain unclear. It has been proposed that when stimulation is first activated, current preferentially travels through high-conductivity sweat glands and hair follicles and this, in turn, leads to pain (Mason and Mackay, 1976; Ledger 1992; Panescu et al., 1994). Over time as electro-osmosis increase the conductivity of the whole skin layer, transdermal current is then distributed more homogenously and pain decreases. Skin electroporation and/or erythema may account, in part, for the accommodation to pain when stimulation is left on, but does not clearly explain the pain spike at the termination of stimulation. Nerve “accommodation” to electric fields may account for the pain spike in the beginning and at the end.
Summary: Toward High-Definition DC stimulation, Potential for Increased Safety
Though fundamental questions remain about the causes of pruritic sensation during transcutaneous DC stimulation, and the role of associated phenomena such as erythema, the initial approach taken in this study indicate that incremental change in electrode design can fundamentally improve stimulation comfort. The observed interface electrochemistry of DC stimulation is explained largely by considering existing theories (Merrill et al., 2005), though the description of a detergible “chemical” insulation layer may be novel. Interface electrochemistry can be mediated through rational selection of electrode materials; moreover, monitoring of electrode potential can be used to indicate a potential for electrochemical product formation. Neither heat nor electrochemical product formation, at least in the bulk gel, simply correlate with sensation, suggesting alternative explanations for pruritis including “funneling” through skin pores and/or direct nerve activation – investigation into these phenomena should support development of still further improved electrode configurations. For the electrode configurations and electrical settings used in the present study: 1) in no cases was skin burned; 2) any pruritic sensations disappeared immediately or rapidly after stimulation was turned off; 3) and any innocuous erythema disappeared within minutes. Thus even under our “worst case” configurations, using our electrode configurations DC current can be applied safely using electrode potential limits (66.7 V) and individual comfort level as end-points. Furthermore, we have no evidence showing that ignoring such end-points would strictly lead to any damage using our electrode designs. Interface electrochemistry is a complex matter and requires additional investigation; similarly, further improvement in durability and tolerability is expected with further advances in design.
It is noteworthy that the use of large electrodes does not inherently prevent skin damage (Leeming et al., 1970; Palm et al., 2008; Lagopoulos and Degabriele, 2008; Bikson et al., 2009a); Firstly, the average current density at a (large electrode), obtained by calculating the total current divided by the total area, underestimates the peak current density at the scalp surface which is inhomogeneous and generally concentrated near the electrode edges (Wiley and Webster, 1982; Prausnitz 1996; Miranda et al., 2009). Thus, using our 12 mm “Ag/AgCl Ring” electrode in combination with an electrolyte gel, the peak current density obtained is not necessarily higher than sponges. For this reason, decreasing the NaCl (electrolyte) content of sponge electrodes may increase comfort (decrease perception) by reducing current density in-homogeneity (even as electrode voltage increases; Dundas 2007). Moreover, using large (sponge) electrodes it becomes increasingly impractical to uniformly control skin contact conditions such as avoiding regions of low-moisture (e.g. following evaporation), uneven gel thickness, or previously damaged skin (Lambert 1995; Lagopoulos and Degabriele, 2008 ), this in turn increases hazards (Schwartz 1989). Finally, increasing electrode area increases the area of skin directly stimulated which (especially if current density is fixed) may increase perception/pain (Martinsen et al., 2004; Prausnitz 1996). Decreasing electrode size does not necessarily increase pain (Forrester and Petrodky 2004). By using relatively small electrodes, it is possible to precisely control stimulation geometry, prevent evaporation, and normalize other factors to mediate comfort and safety. In addition to facilitating more targeted stimulation (e.g. 4X1 configuration; Datta et al., 2009a), even when diffuse areas of the brain are targeted, a closely spaced array of smaller electrodes may be preferred. For example, an array of high-definition electrodes can be arranged in a square (e.g. 4X4 configuration) and connected electrically in parallel, substituting sponge electrodes. Multicenter clinical trials using high-definition electrodes are currently ongoing. Critically, as high-lighted throughout this report, the design of the entire electrode assembly must be carefully designed and validated.
Supplementary Material
Acknowledgments
The authors are grateful for the technical assistance and overall expertise provided by Thomas Radman of the City College of New York. This work was supported in part by the Wallace H Coulter foundation, a P.S.C. CUNY Grant, The Andy Grove Foundation, and NIH-NCI.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Agnew AF, McCreery DB. Considerations for safety in the use of extracranial stimulation for motor evoked potentials. Neurosurgery. 1987;20:143–147. doi: 10.1097/00006123-198701000-00030. [DOI] [PubMed] [Google Scholar]
- 2.Berliner MN. Skin microcirculation during Tapwater Iontophoresis in humans: cathode stimulates more than anode. Microvasc Res. 1997;54(1):74–80. doi: 10.1006/mvre.1997.2025. [DOI] [PubMed] [Google Scholar]
- 3.Bikson M, Bulow P, Stiller JW, Datta A, Battaglia F, Karnup SV, Postolache TT. Transcranial direct current stimulation for major depression: a general system for quantifying transcranial electrotherapy dosage. Curr Treat Options Neurol. 2008;10:377–385. doi: 10.1007/s11940-008-0040-y. [DOI] [PubMed] [Google Scholar]
- 4.Bikson M, Datta A, Elwassif M. Establishing safety limits for transcranial direct current stimulation. Clinical Neurophysiology. 2009a;120:1033–1034. doi: 10.1016/j.clinph.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bikson M, Datta A, Elwassif M, Bansal V, Peterchev AV. Introduction to electrotherapy technology. J Pain Management. 2009b;2(3):231–238. [Google Scholar]
- 6.Roth Bradley J. What does the ratio of injected current to electrode area not tell us about tDCS? Clinical Neurophysiology. 2009;120(6):1037–1038. doi: 10.1016/j.clinph.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Craane-van Hinsberg WHM, Verhoef JC, Junginger HE, Boddé HE. Thermoelectrical analysis of the human skin barrier. Thermochimica Acta. 1995;248:303–318. [Google Scholar]
- 8.Cooper JB, DeCesare R, D'Ambra MN. An Engineering Critical Incident: Direct Current Burn from a Neuromuscular Stimulator. Anesthesiology. 1990;73:168–172. doi: 10.1097/00000542-199007000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Droog EJ, Sjoberg F. Nonspecific vasodilation during transdermal iontophoresis – the effect of voltage over skin. Macrovascular Research. 2003;65:172–178. doi: 10.1016/s0026-2862(03)00002-5. [DOI] [PubMed] [Google Scholar]
- 10.Datta A, Elwassif M, Battaglia F, Bikson M. Transcranial current stimulation focality using disc and ring electrode configurations: FEM analysis. J Neural Eng. 2008;5:163–174. doi: 10.1088/1741-2560/5/2/007. [DOI] [PubMed] [Google Scholar]
- 11.Datta A, Bansal V, Diaz J, Patel J, Reato D, Bikson M. Gyri-precise head model of transcranial DC stimulation: Improved spatial focality using a ring electrode versus conventional rectangular pad. Brain Stimulation. 2009a;2(4):201–207. doi: 10.1016/j.brs.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Datta A, Elwassif M, Bikson M. Bio-heat transfer model of transcranial DC stimulation: Comparison of conventional pad versus ring electrode. Conf Proc IEEE Eng Med Biol Soc. 2009b Sept 3–6;:670–673. doi: 10.1109/IEMBS.2009.5333673. [DOI] [PubMed] [Google Scholar]
- 13.Dundas JE, Thickbroom GW, Mastaglia FL. Perception of comfort during transcranial DC stimulation: Effect of NaCl solution concentration applied to sponge electrodes. Clinical Neurophysiology. 2007;118:1166–1170. doi: 10.1016/j.clinph.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 14.Gilad O, Horesh L, Holder DS. Design of electrodes and current limits for low frequency electrical impedance tomography of the brain. Med Biol Eng Comput. 2007;45:621–633. doi: 10.1007/s11517-007-0209-7. [DOI] [PubMed] [Google Scholar]
- 15.Geddes LA, Roeder RA. Direct-current injury: Electrochemical aspects. Journal of clinical monitoring and computing. 2004;18(3):157–61. doi: 10.1023/b:jocm.0000042923.00392.a8. [DOI] [PubMed] [Google Scholar]
- 16.Kiernan MC, Guglielmi JM, Kaji R, Murray NM, Bostock H. Evidence for axonal membrane hyperpolarization in multifocal motor neuropathy with conduction block. Brain. 2002;125:664–675. doi: 10.1093/brain/awf041. [DOI] [PubMed] [Google Scholar]
- 17.Lagopoulos J, Degabriele R. Feeling the heat: the electrode-skin interface during DCS. Acta Neuropsychiatrica. 2008;20:98–100. [Google Scholar]
- 18.Lambert H, De Bartselier E, Vanalme G, De Mey G. Skin burn risks using transcutaneous direct current. Engineering in Medicine and Biology Society. 1995;1:647–648. [Google Scholar]
- 19.Leach EH, Peters RA, Rossiter RJ. Experimental thermal burns, especially the moderate temperature burn. Exp physiol. 1943;32:67–86. [Google Scholar]
- 20.Ledger, Philip W. Skin biological issues in electrically enhanced transdermal delivery. Advanced Drug Delivery Reviews. 1992;9:289–307. [Google Scholar]
- 21.Leeming MN, Ray C, Jr, Howland WS. Low-Voltage Direct Current Burns. JAMA. 1970;214:1681–1684. [PubMed] [Google Scholar]
- 22.Liebetanz D, Koch R, Mayenfels S, Koniq F, Paulus W, Nitsche MA. Safety limits of cathodal transcranial direct current stimulation in rats. Clinical Neurophysiology. 2009;120(6):1161–1167. doi: 10.1016/j.clinph.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 23.Martin GT, Pliquett UF, Weaver JC. Theoretical analysis of localized heating in human skin subjected to high voltage pulses. Bioelectrochemistry. 2002;57(1):55–64. doi: 10.1016/s1567-5394(01)00176-1. [DOI] [PubMed] [Google Scholar]
- 24.Martinsen OG, Grimnes S, Piltan H. Cutaneous perception of electrical direct current. ITBM–RBM. 2004;25 (4):240–243. [Google Scholar]
- 25.McCreery DB, Agnew WF, Yuen TG, Bullara L. Charge Density and Charge Per Phase as Cofactors in Neural Injury Induced by Electrical Stimulation. IEEE Trans Biomed Eng. 1990;37(10):996–1001. doi: 10.1109/10.102812. [DOI] [PubMed] [Google Scholar]
- 26.Merrill DR, Bikson M, Jefferys JGR. Electrical stimulation of excitable tissue: design of efficacious and safe protocols. J Neuro Meth. 2005;141:171–198. doi: 10.1016/j.jneumeth.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Miranda P, Faria P, Hallett M. What does the ratio of injected current to electrode area tell us about tDCS efficacy? Brain Stimulation. 2008;1(3):269. [Google Scholar]
- 28.Miranda P, Faria P, Hallett M. What does the ratio of injected current to electrode area tell us about current density in the brain during tDCS? Clinical Neurophysiology. 2009;120(6):1183–1187. doi: 10.1016/j.clinph.2009.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Molitor H, Fernandez L. Experimental Studies on the causes and prevention of iontophoretic burns. Am J Med Sci. 1939;198:778–785. [Google Scholar]
- 30.Nitsche MA, Liebetaz D, Lang N, et al. Safety criteria for transcranial direct current stimulation (tDCS) in humans. Clinical Neurophysiology. 2003;114:2220–2222. doi: 10.1016/s1388-2457(03)00235-9. [DOI] [PubMed] [Google Scholar]
- 31.Nitsche MA, Doemkes S, Karakose T. Shaping the effects of transcranial direct current stimulation of the human motor cortex. J Neurophysiol. 2007;97:3109–3117. doi: 10.1152/jn.01312.2006. [DOI] [PubMed] [Google Scholar]
- 32.Nitsche M, Cohen L, Wassermann E, Priori A, Lang N, Antal A, Paulus W, Hummel F, Boggio P, Fregni F. Transcranial direct current stimulation: State of the art 2008. Brain Stimulation. 2008;1:206–223. doi: 10.1016/j.brs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Palm U, Keeser D, Schiller C, Fintescu Z, Reisinger E, Padberg F, Nitsche M. Skin lesions after treatment with transcranial direct current stimulation (tDCS) Brain Stimulation. 2008;1:386–387. doi: 10.1016/j.brs.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 34.Panescu D, Webster JG, Stratbucker RA. A nonlinear finite element model of the electrode-electrolyte-skin system. Biomedical Engineering, IEEE Transactions on. 1994;41(7):681–687. doi: 10.1109/10.301735. [DOI] [PubMed] [Google Scholar]
- 35.Pliquett UF, Martin GT, Weaver JC. Kinetics of the temperature rise within human stratum corneum during electroporation and pulsed-high-voltage iontophoresis. Biochemistry. 2002;57:65–72. doi: 10.1016/s1567-5394(01)00177-3. [DOI] [PubMed] [Google Scholar]
- 36.Poletto CJ, Van Doren CL. A high voltage, constant current stimulator for electrocutaneous stimulation through small electrodes. Biomedical Engineering, IEEE Transactions on. 1999;46(8):929–936. doi: 10.1109/10.775402. [DOI] [PubMed] [Google Scholar]
- 37.Poreisz C, Boros K, Antal A, Paulus W. Safety aspects of transcranial direct current stimulation concerning healthy subjects and patients. Brain Res Bull. 2007;72:208–214. doi: 10.1016/j.brainresbull.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Prausnitz MR. The effects of electric current applied to skin: A review for transdermal drug delivery. Advanced Drug Delivery Reviews. 1996;18:395–425. [Google Scholar]
- 39.Swartz CM. Safety and ECT stimulus Electrodes: II. Clinical Procedures. 1989;5(2):176–179. [PubMed] [Google Scholar]
- 40.Swartz CM. Safety and ECT Stimulus Electrode: I. Heat Liberation at the Electrode-Skin Interface Convulsive Therapy. 1989;5(2):171–175. [PubMed] [Google Scholar]
- 41.Tallgren P, Vanhatallo S, Kaile K, Voipio J. Evaluation of commercially available electrodes and gels for recording of slow EEG potentials. Clinical Neurophysiology. 2005;116(4):799–806. doi: 10.1016/j.clinph.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 42.Wiley JD, Webster JG. Distributed Equivalent-Circuit Models for Circular Dispersive electrodes. IEEE Trans Biomed Eng. 1982;29(5):385–389. doi: 10.1109/TBME.1982.324911. [DOI] [PubMed] [Google Scholar]
- 43.Yuen TGH, Agnew WF, Bullara LAB, Skip Jaques BS, McCreery DB. Histological evaluation of neural damage from electrical stimulation: considerations for the selection of parameters for clinical application. Neurosurgery. 1981;9:292–299. [PubMed] [Google Scholar]
- 44.Yoshida K, Patriciu A. Changes in the Skin and Electrode Impedance Spectra due to Long Term Surface Stimulation. Proc Fifth Annual IFESS Conference. 2000;5:282–284. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.