Abstract
The homeostatic iron regulator protein HFE is involved in regulation of iron acquisition for cells. The prevalence of two common HFE gene variants (H63D, C282Y) has been studied in many cancer types; however, the impact of HFE variants, sex and HFE gene expression in lung cancer has not been studied. We determined the prevalence of HFE variants and their impact on cancer phenotypes in lung cancer cell lines, in lung cancer patient specimens, and using The Cancer Genome Atlas (TCGA) database. We found that seven out of ten human lung cancer cell lines carry the H63D or C282Y HFE variant. Analysis of lung cancer specimens from our institute (Penn State Hershey Medical Center) revealed a sex and genotype interaction risk for metastasis in lung adenocarcinoma (LUAD) patients; H63D HFE is associated with less metastasis in males compared to wild type (WT) HFE; however, females with the H63D HFE variant tend to develop more metastatic tumors than WT female patients. In the TCGA LUAD dataset, the H63D HFE variant was associated with poorer survival in females compared to females with WT HFE. The frequency of C282Y HFE is higher in female lung squamous cell carcinoma (LUSC) patients of TCGA than males, however the C282Y HFE variant did not impact the survival of LUSC patients. In the TCGA LUSC dataset, C282Y HFE patients (especially females) had poorer survival than WT HFE patients. HFE expression level was not affected by HFE genotype status and did not impact patient’s survival, regardless of sex. In summary, these data suggest that there is a sexually dimorphic effect of HFE polymorphisms in the survival and metastatic disease in lung cancer.
Introduction
Lung cancer is the second most common cancer in both men and women and is the leading cause of cancer deaths in the US [1]. There are two types of lung cancers: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC is the most common type of lung cancer and accounts for approximately 80–85% of lung cancers [2–4]. There are 3 main types of NSCLC: adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Adenocarcinoma, the most common form of lung cancer in non-smokers, accounts for about 40% of all lung cancers. Squamous cell carcinoma accounts for roughly 30% and large cell carcinoma is less than 10%. SCLC accounts for ~20% of all lung cancers, with a 5-year survival of only 5–10% [4, 5]. Molecular profiling of NSCLC found higher gene mutations in multiple oncogenes, such as epidermal growth factor receptor (EGFR) (10–35%), K-ras (KRAS) (15–25%), and Phosphatase and tensin homolog (PTEN) (4–8%). Other gene alterations, e.g. Fibroblast growth factor receptor 1 (FGFR1) amplification (20%) and anaplastic lymphoma kinase (ALK) rearrangement (3–7%) are also found in NSCLC [6–8]. Interestingly, many driver mutations found in lung adenocarcinoma (LUAD) are rarely found in lung squamous cell carcinoma (LUSC), which suggests distinct cancer development processes among lung cancer sub-types.
Cancer cells have a robust iron appetite associated with their higher growth and metabolism [9]. Iron can influence the epigenetics of cancer cells [10] and the tumor microenvironment by impacting macrophage function [11, 12]. Among the many iron metabolism genes, the HFE (homeostatic iron regulator) gene has been interrogated for its relationship to cancer. The HFE gene encodes for a 343-amino acid major histocompatibility complex (MHC) class 1 molecule [13] whose interaction with the transferrin receptor (TFRC) on the cell membrane regulates the amount of iron internalized to the cell by limiting the interaction of transferrin (TF) with the TFRC. The HFE gene contains genetic polymorphisms identified as risk factors or disease modifiers for several human diseases such as hereditary hemochromatosis, neurodegenerative diseases, liver disease, and cancers [14–18].
Polymorphisms in the HFE gene occur more frequently in Caucasians than in other races [19–21]. There are two major mutation sites in the HFE gene [13]. One is H63D, a single mutation of C to G at nucleotide 187, which results in a substitution of aspartate for histidine at amino acid 63. The other one is C282Y, a mutation of G to A at nucleotide 845, which results in the substitution of tyrosine for cysteine at amino acid 282. In the normal Caucasian population, the frequency of H63D and C282Y HFE genotype is around 26% (24% heterozygote and 2.4% homozygote) and 10% (10% heterozygote and 0.44% homozygote), respectively [19]. The allelic frequency of H63D and C282Y HFE in the general Caucasian population is 15.3% and 6.8% [20]. Increased frequency of the HFE variants have been reported in acute lymphoblastic leukemia [22, 23] and breast cancer [24, 25]. Increased frequency of H63D HFE variant was observed in malignant gliomas [26]. The H63D HFE variant is also a risk factor for colorectal cancer [27], hepatocellular carcinoma [28–30], and pancreatic cancer [30, 31]. Increased frequency of C282Y HFE variant was observed in colorectal cancer [32] and hepatocellular carcinoma [33]. In addition, the C282Y HFE variant is a risk factor for breast cancer [31, 34, 35], colorectal cancer [34, 35], hepatocellular carcinoma [30, 31, 35, 36], liver cancer [37], and ovarian cancer [38]. The risk of C282Y HFE variant in colorectal cancer has been reported as both increased [32] and decreased [31]. In our previous study using Penn State Health Milton S. Hershey Medical Center (PSHMC) glioblastoma (GBM) patient’s samples, we demonstrated poorer overall survival in male GBM patients with H63D HFE than male WT HFE GBM patients [39] although this finding was not observed in TCGA GBM samples [40].
Despite the prevalence of lung cancer and the prevalence of the HFE gene variants, the impact of HFE genotype on lung cancer has not been studied systematically and this knowledge gap is addressed in this study. We interrogated the HFE genotype and/or HFE expression in human lung cancer cell lines, specimens of lung cancer patients, and lung cancer database.
Materials and methods
Cell culture
All tested lung cancer cell lines were ordered from American Type Culture Collection (ATCC, Manassas, VA) or obtained from Dr. Jong K. Yun (Pennsylvania State University College of Medicine). Human lung cancer cell lines were maintained in Roswell Park Memorial Institute (RPMI) media 1640 with 1X Penicillin-Streptomycin and 10% fetal bovine serum (FBS). RPMI media 1640 and other cell culture ingredients were purchased from Life Technologies (Grand Island, NY).
HFE genotype of cell lines and plasma of lung cancer patients at the Penn State Health Milton S. Hershey Medical Center (PSHMC)
HFE genotype of lung cancer cell lines was determined using a restriction enzyme digestion method after PCR. The digested PCR products were run in 5% TBE polyacrylamide gel for HFE genotype as reported [41]. The HFE genotyping from plasma of lung cancer patients was performed using same method after genomic DNA purification using DNeasy Tissue kit (Qiagen) according to the manufacturer's instructions. The HFE genotype of select samples was confirmed via DNA sequencing.
The de-identified plasma samples and clinical data of human lung cancer patients were obtained from Tumor Bank of Penn State Institute for Personalized Medicine (PSIPM) and approved by Penn State College of Medicine Institutional Review Board (IRB Protocol Number 40532). DNA was purified from the plasma samples by DNeasy Blood & Tissue kit (QIAAGEN) to determine HFE genotype as described above. For HFE genotype data analysis, we used only Caucasian lung cancer patients’ samples, because HFE polymorphisms are most prevalent in the Caucasian population. We consented and enrolled 53 adenocarcinoma of the lung (23 male and 30 female) and 41 squamous cell lung cancer patients (28 male and 13 female).
The HFE genotype of lung cancer patients was compared with samples from individuals without cancer or with neurological disease in our Institute of Personalized Medicine [41] and 1000Genome data which was downloaded the frequency of Single Nucleotide Variants (SNVs) in the HFE gene using Variant Call Format (VCF) file from The International Genome Sample Resource.
The Cancer Genome Atlas (TCGA) lung cancer patient’s data
There are two types of lung cancer data in the TCGA database: lung adenocarcinoma (LUAD) and lung squamous cell carcinoma (LUSC). In the TCGA lung cancer database, we used two samples data from each lung cancer patients. i.e., Blood Derived Normal (NB), Primary Solid Tumor (TP). The total number of NB samples of LUAD patients with corresponding HFE genotype information was 408. Among 408 samples, there were 307 Caucasian, 36 Black, 6 Asian, and 59 unknown. The total number of TP samples of LUAD patients who had HFE genotype information was 558. Among the 558 samples, there were 381 Caucasian, 52 Black, 8 Asian, 1 American Indian, and 116 unknown. The total number of NB samples of LUSC patients who had HFE genotype information was 322. Among 322 samples, there were 203 Caucasian, 15 Black, 6 Asian, and 98 unknown. The total number of TP samples of LUSC patients who had HFE genotype information was 507. Among 507 samples, there were 300 Caucasian, 28 Black, 9 Asian, and 170 unknown. We accessed HFE gene variant data from Cancer Genomics Hub (CGHub) using GeneTorrent and GTFuse software (AnnaiSystems, Carlsbad, CA) to extract and download only HFE genes from complete mapped sequence (BAM) files. Genome Analysis Toolkit (GATK) software, based on the GATK best practices pipeline, was used to identify HFE gene variants (H63D, C282Y) from the sequences as we previously reported [40]. Clinical data for the TCGA lung adenocarcinoma and lung squamous cell carcinoma cohorts was accessed with TCGA biolinks [42–44]. During our TCGA lung cancer data analysis, we noticed that some patients had extremely short follow-up times (< 30 days). Because we were concerned that these short survival times could bias the results of our survival analyses, we performed HFE genotype status and survival analyses using either (i) all subjects, or (ii) all subjects with follow-up times greater than 30 days (both living and deceased). The two approaches produced highly concordant results. Therefore, the results presented here are based on an analysis of all patients.
Association between HFE genotype/HFE expression/Sex and survival in TCGA lung cancer patients
RNA sequencing (RNA-Seq) and clinical data from the TCGA LUAD and LUSC cohorts were accessed from the Broad Institute’s Firehose GDAC (https://gdac.broadinstitute.org/). We applied a log transformation to the resulting normalized RSEM (RNA-Seq by Expectation-Maximization) values from RNA-Seq, so gene expression was quantified as log2 (RSEM + 1). Primary tumor samples (LUAD, n = 515; LUSC, n = 445) and matched patient’s normal samples (LUAD, n = 58; LUSC, n = 33) were identified from the TCGA barcodes. Kruskal-Wallis tests or Wilcoxon rank sum tests were used to compare HFE expression values in the following groups: (i) HFE variant vs. HFE wild type (WT), (ii) females vs. males. Separate analyses were performed for primary tumor and matched blood samples in each subject. Additionally, H63D and C282Y variants were considered separately in each tumor type, and the variant status for matched normal samples was determined by the status of the matched primary tumor sample. Kaplan-Meier plots and log rank tests were applied to compare survival times in groups defined by HFE expression level. Survival times were compared for females and males after defining HFE expression groups as high or low based on median expression or based on quartiles. Additionally, multivariable Cox proportional hazards models were fit using either HFE genotype or HFE expression while adjusting for tumor stage (early stage (I/II) vs. advanced stage (III/IV)), age at diagnosis, gender, and smoking (never smoked vs. any smoking history). All survival analyses were performed after restricting to Caucasians only.
Statistical analysis
Comparisons of HFE gene variant frequency between samples were determined using Fisher‘s exact test or Chi-square test. Additionally, the associations between HFE gene variant and sex were examined using Fisher’s exact test. The association between patients’ overall survival and HFE polymorphisms (H63D, C282Y) was indicated by Kaplan-Meier survival curve and analyzed by log-rank test. The log-rank test results were further examined using multi-variable Cox proportional hazards regression models, by controlling for several known confounders. R 3.5.0 (R Foundations) was used to conduct all data analyses for HFE expression related study [45], and the survival analyses were performed using the survival R package [46] and GraphPad Prism 7 software. All tests were two-sided and the statistical significance level was set to 0.05.
Results
HFE genotype of lung cancer cell lines
Of the ten lung cancer cell lines investigated, 6 expressed the H63D HFE variant and 1 had the C282Y HFE variant (Table 1). Only 1 large cell lung cancer cell line did not have a HFE gene variant and the only squamous cell carcinoma cell line was heterozygote for C282Y.
Table 1. HFE genotype of lung cancer cell lines.
| Name | Tissue or cancer type | Stage | H63D HFE | C282Y HFE |
|---|---|---|---|---|
| A549 | Carcinoma | NA | hetero | wildtype |
| H23 | Adenocarcinoma, Non-small cell lung cancer | NA | hetero | wildtype |
| H441 | Papillary adenocarcinoma | NA | hetero | wildtype |
| H460 | Carcinoma; large cell lung cancer | NA | wildtype | wildtype |
| H520 | Squamous cell carcinoma | NA | wildtype | hetero |
| H522 | Adenocarcinoma, Non-small cell lung cancer | 2 | hetero | wildtype |
| H838 | Adenocarcinoma, Non-small cell lung cancer | 3B | wildtype | wildtype |
| H1299 | Carcinoma, Non-small cell lung cancer | NA | wildtype | wildtype |
| H1650 | Adenocarcinoma; bronchoalveolar carcinoma | 3B | hetero | wildtype |
| H1993 | Lung adenocarcinoma | 3A | homo | wildtype |
NA (not available); hetero (heterozygote); homo (homozygote)
Frequency of HFE genotype in lung cancer patients
We determined the frequency of HFE gene variants in lung cancer patients (adenocarcinoma of the lung, squamous cell lung cancer) seen in our Penn State Hershey Medical Center (PSHMC), and publically available lung cancer databases. The characteristics of lung cancer patients, such as median age, age range, and male: female ratio, are summarized in Table 2.
Table 2. Characteristics of our study sample, TCGA lung cancer, and 1000Genome data.
| PSHMC LUAD (n = 53) | PSHMC LUSC (n = 41) | TCGA LUAD_NB (n = 307) | TCGA LUAD_TP (n = 381) | TCGA LUSC_NB (n = 203) | TCGA LUSC_TP (n = 300) | PSHMC Non-cancer (n = 94) a | White in 1000Genome Phase 3 (n = 185) b | |
|---|---|---|---|---|---|---|---|---|
| Median age (years old) | 70, (Male: 71; Female: 68.5) |
73, (Male: 73; Female: 70) |
67, (Male: 66.5; Female: 67) |
67, (Male: 66.5; Female: 67) |
68, (Male: 68; Female: 69.5) |
68, (Male: 68; Female: 69) |
58, (Male: 61; Female: 56) |
NA |
| Range of age (years old) | 48–90, (Male: 54–84; Female: 48–90) | 40–84, (Male: 54–81; Female: 40–84) | 33–88, (Male: 38–88; Female: 33–87) | 33–88, (Male: 38–88; Female: 33–87) | 44–85, (Male: 46–85; Female: 44–83) | 40–85, (Male: 40–85; Female: 44–83) | 40–85, (Male: 41–82; Female: 40–85) | NA |
| Male : Female (ratio) | 23 : 30 (1 : 1.3) | 28 : 13 (2.15: 1) | 140 : 167 (1 : 1.2) | 172 : 209 (1 : 1.2) | 151 : 52 (2.9 : 1) | 219 : 81 (2.7 : 1) | 34 : 60 (1 : 1.8) | 80 : 102 (1 : 1.3) |
LUAD (lung adenocarcinoma)
LUSC (lung squamous cell carcinoma)
NB (blood normal)
TP (tumor patient)
aLee SY et al. PLoS One. 2017;12(3):e0174778. [40]
bThere are a total of 1,077 samples (527 male, 550 female) listed on the website, however, only a subset have sequences. There are 185 European subpopulation (80 male, 102 female, 3 unknown). Age information is not available.
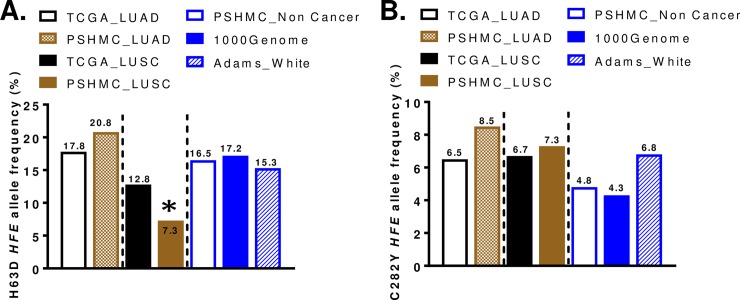
We limited our analysis to Caucasians because of the higher frequency of HFE polymorphisms compared to other races [19–21]. Among 53 lung adenocarcinoma patients in PSHMC, the frequency of H63D and C282Y HFE gene variant was 32.0% and 13.2%, respectively (S1 Table). In squamous cell lung cancer patients, the frequency of H63D and C282Y HFE variant was 14.6% and 12.2%, respectively (S1 Table). The allele frequency of H63D HFE was 20.8% and 8.5% for C282Y HFE in lung adenocarcinoma, and 7.3% for H63D HFE and 7.3% for C282Y HFE in lung squamous cell carcinoma. Statistical analysis revealed a lower frequency of H63D HFE alleles in squamous cell carcinoma compared to adenocarcinoma (p = 0.007). In comparison to non-cancer population adenocarcinoma tended to have higher C282Y HFE allele frequency (p = 0.08) compared to 1000Genome database. Squamous cell carcinoma had significantly lower H63D HFE allelic frequency than the PSHMC control samples (p = 0.0336) or 1000Genome data (p = 0.04).
There were no differences between TCGA lung cancer samples (LUAD, LUSC) and non-cancer population for the frequency of HFE genotype or HFE alleles (S2 Table). The summary of allele frequencies for H63D HFE and C282Y HFE in lung cancers and controls are summarized in Fig 1.
Fig 1. Allele frequency of HFE variants in lung cancers and control population (non-cancer general population).
(A) H63D HFE allele frequency in the blood samples of lung cancer patients (TCGA LUAD or LUSC, PSHMC) and non-cancer control (PSHMC non-cancer, 1000Genome, and White of Adams study in 2005 [20]). The asterisk (*) indicates significantly decreased H63D HFE allele frequency in LUSC of PSHMC patients compared to non-cancer control population. p<0.05 (B) C282Y HFE allele frequency in the blood samples of lung cancer patients (TCGA LUAD or LUSC, PSHMC) and general population (PSHMC non-cancer, 1000Genome, and White of Adams study in 2005 [20]).
Association between HFE genotype and sex in the lung cancer patients
Because distinct male: female ratios exist in two lung cancer types (lung adenocarcinoma, lung squamous cell carcinoma), the HFE genotype data were stratified by sex. There was an increase in the C282Y HFE allelic frequency in female LUAD patients in the TCGA database (p = 0.0474) (Table 3) but not in the PSHMC database (S3 Table). There were no sex differences in the H63D HFE allele groups.
Table 3. Frequency of HFE genotype and alleles based on sex in TCGA lung cancer (Caucasian patients).
| TCGA LUAD | TCGA LUSC | |||||||
|---|---|---|---|---|---|---|---|---|
| NB (n = 307) | TP (n = 381) | NB (n = 203) | TP (n = 300) | |||||
| Male (n = 140) | Female (n = 167) | Male (n = 172) | Female (n = 209) | Male (n = 151) | Female (n = 52) | Male (n = 219) | Female (n = 81) | |
| Genotype | ||||||||
| H63/D63 (heterozygote) | 37 (26.4%) | 46 (27.5%) | 41 (23.8%) | 57 (27.3%) | 32 (21.2%) | 13 (25.0%) | 46 (21.0%) | 20 (24.7%) |
| D63/D63 (homozygote) | 6 (4.3%) |
7 (4.2%) |
6 (3.5%) |
8 (3.8%) |
3 (2.0%) |
1 (1.9%) |
7 (3.2%) |
3 (3.7%) |
| C282/Y282 (heterozygote) | 12 (8.6%) |
22 (13.2%) | 14 (8.1%) | 30 (14.4%) | 20 (13.2%) | 5 (9.6%) |
27 (12.3%) | 5 (6.2%) |
| Y282/Y282 (homozygote) | 0 (0.0%) | 3 (1.8%) | 1 (0.6%) | 2 (1.0%) | 0 (0.0%) | 1 (1.9%) | 0 (0.0%) | 1 (1.2%) |
| Alleles | ||||||||
| H63D HFE | 49/280 (17.5%) | 60/334 (18.0%) | 53/344 (15.4%) | 73/418 (17.5%) | 38/302 (12.6%) | 15/104 (14.4%) | 60/438 (13.7%) | 26/162 (16.1%) |
| C282Y HFE | 12/280 (4.3%) | 28/334 (8.4%) | 16/344 (4.7%) | 34/418 (8.1%) | 20/302 (6.6%) | 7/104 (6.7%) | 27/438 (6.2%) | 7/162 (4.3%) |
| Fisher’s exact test (Male vs. Female) | p = 0.9142 (H63D) p = 0.0474 (C282Y) |
p = 0.4268 (H63D) p = 0.0549 (C282Y) |
p = 0.6082 (H63D) p = 1.0 (C282Y) |
p = 0.4249 (H63D) p = 0.4308 (C282Y) |
||||
Values were expressed as n = N (%)
LUAD (lung adenocarcinoma)
LUSC (lung squamous cell carcinoma)
NB (blood normal)
TP (tumor patient)
Association between HFE genotype and HFE expression and sex in TCGA lung cancer data (Caucasian patients)
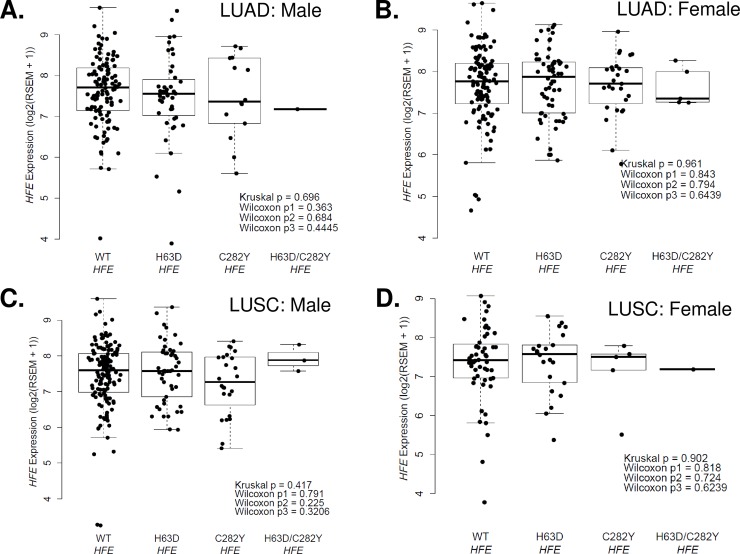
We evaluated the association between HFE genotype and HFE mRNA expression in TCGA lung cancer data. There were no differences between WT and H63D or C282Y HFE variants in matched normal or primary tumors of LUAD and LUSC lung cancer patients in two sample t-test (S1 and S2 Figs). The level of HFE expression was not different between males and females in matched normal or primary tumors of LUAD and LUSC lung cancer patients in two sample t-test (S1 and S2 Figs). There were no HFE expression differences between WT and HFE variants in male or female LUAD and LUSC in the TCGA lung cancer dataset (Fig 2).
Fig 2. Association between HFE expression and HFE genotype or sex in TCGA lung cancer data.
(A) HFE gene expression based on HFE genotype (WT, H63D, C282Y, H63D and C282Y) in male primary tumor LUAD patients. (B) HFE gene expression based on HFE genotype (WT, H63D, C282Y, H63D and C282Y) in female primary tumor LUAD patients. (C) HFE gene expression based on HFE genotype (WT, H63D, C282Y, H63D and C282Y) in male primary tumor LUSC patients. (D) HFE gene expression based on HFE genotype (WT, H63D, C282Y, H63D and C282Y) in female primary tumor LUSC patients. Kruskal p = the p-value for the Kruskal-Wallis test comparing the median HFE expression levels in each of the four groups, Wilcox p1 = the p-value for the Wilcoxon rank sum test comparing the median HFE expression levels in WT HFE vs. H63D HFE, Wilcox p2 = the p-value for the Wilcoxon rank sum test comparing the median HFE expression levels in WT HFE vs. C282Y HFE, Wilcox p3 = the p-value for the Wilcoxon rank sum test comparing the median HFE expression levels in WT HFE vs. H63D/C282Y HFE.
Impact of HFE genotype on the metastasis of lung cancer patients at PSHMC
Metastatic disease was only available in the PSHMC database. The incidence of metastasis in lung cancer patients at PSHMC revealed no statistical difference between WT and HFE polymorphisms but when we stratified for sex, there were significant differences between WT and HFE polymorphisms (Table 4). None of the H63D HFE male adenocarcinoma patients developed metastases while 50% of WT HFE male patients did (p = 0.0189); whereas in females the findings were opposite with H63D HFE carriers tending to develop more metastases than WT HFE (p = 0.0596). With the C282Y HFE variant, male adenocarcinoma patients tend to develop more metastases compared to WT HFE male carriers (p = 0.0672) while there is no difference in females. In squamous cell lung cancer, neither of the HFE variants (H63D and C282Y) or sex impacted metastatic rate.
Table 4. HFE genotype and metastasis rate based on sex of lung cancer patients at PSHMC.
| Male |
PSHMC LUAD (n = 23), n (%) |
Metastasis, n (%) | Fisher’s exact test (WT HFE vs variant HFE) | PSHMC LUSC (n = 28), n (%) | Metastasis, n (%) | Fisher’s exact test (WT HFE vs variant HFE) | |
| H63D HFE | CC | 14 (60.9%) | 7 (50.0%) | p = 0.0189 | 24 (85.7%) | 10 (41.7%) | p = 0.0978 |
| CG or GG | 9 (39.1%) | 0 (0.0%) | 4 (16.7%) | 4 (100.0%) | |||
| C282Y HFE | GG | 19 (82.6%) | 4 (21.1%) | p = 0.0672 | 24 (85.7%) | 11 (45.8%) | p = 0.5956 |
| GA or AA | 4 (17.4%) | 3 (75.0%) | 4 (16.7%) | 3 (75.0%) | |||
| Female | LUAD (n = 30), n (%) | Metastasis, n (%) | Fisher’s exact test (WT HFE vs variant HFE) | LUSC (n = 13), n (%) | Metastasis, n (%) | Fisher’s exact test (WT HFE vs variant HFE) | |
| H63D HFE | CC | 22 (73.3%) | 3 (13.6%) | p = 0.0596 | 11 (84.6%) | 2 (18.2%) | p = 1.0 |
| CG or GG | 8 (26.7%) | 4 (50.0%) | 2 (15.4%) | 0 (0.0%) | |||
| C282Y HFE | GG | 27 (90.0%) | 7 (25.9%) | p = 1.0 | 12 (92.3%) | 2 (16.7%) | p = 1.0 |
| GA or AA | 3 (10.0%) | 0 (0.0%) | 1 (7.7%) | 0 (0.0%) | |||
LUAD (lung adenocarcinoma)
LUSC (lung squamous cell carcinoma)
Association between HFE genotype/HFE expression/Sex and patient survival in lung cancer patients at PSHMC and TCGA lung cancer data
There was no survival difference between WT and H63D HFE (p = 0.2866 for LUAD; p = 0.3740 for LUSC), or WT and C282Y HFE (p = 0.6568 for LUAD; p = 0.2498 for LUSC) lung cancer patients who enrolled at PSHMC (S3 Fig).
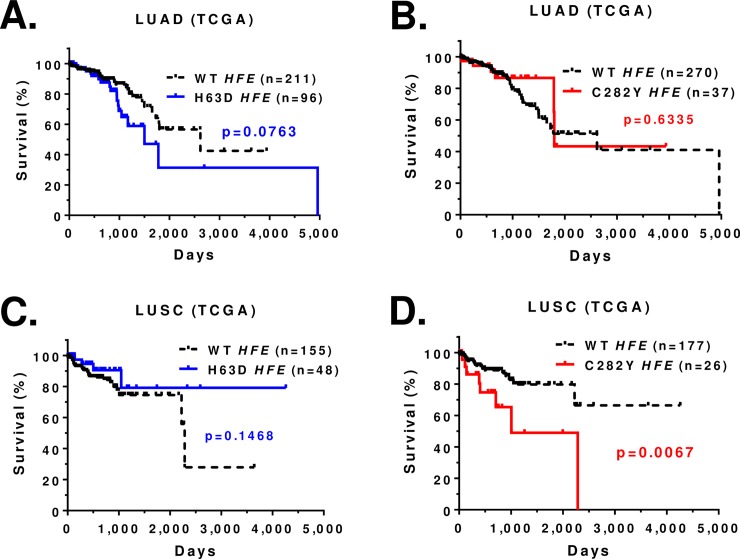
In TCGA database, the Kaplan-Meier survival curve for lung adenocarcinoma patients showed a trend toward poorer survival in H63D HFE variants compared to WT HFE patients (p = 0.0763) (Fig 3A). When the analysis focused on H63D homozygotes compared to WT HFE patients, the survival difference was marginally significant (p = 0.0539) (S4A Fig). The survival for WT HFE patients and C282Y HFE patients was not different (Fig 3B). The Kaplan-Meier survival curve for LUSC patients revealed a significant survival difference between WT HFE patients and C282Y HFE patients (p = 0.0067), but not between WT HFE and H63D HFE variants (Fig 3C and 3D).
Fig 3. Kaplan-Meier survival curve for TCGA lung cancer patients (Caucasians) with HFE genotype.
(A) Survival curve of LUAD patients with WT or H63D HFE. (B) Survival curve of LUAD patients with WT or C282Y HFE. (C) Survival curve of LUSC patients with WT or H63D HFE. (D) Survival curve of LUSC patients with WT or C282Y HFE. Statistical analysis was performed by log-rank test and indicated as p value. Censored record is indicated as + in the graph.
We performed multiplex Cox regression to double check the bivariate associations (Kaplan-Meier curve) between HFE gene variant and overall survival by further controlling other possible factors (tumor stage etc.) that could contribute to the overall survival. The effect of C282Y HFE variant on LUSC patient survival remains significant after controlling for age, tumor stage, and smoking status in multiple Cox regression (Table 5).
Table 5. Hazard ratios from the multiple-variable Cox model for the TCGA lung cancer (Caucasian patients).
| Multivariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|
| HR | P-value | HR | P-value | ||
| LUAD: | |||||
| H63D variant | 0.71 (0.38–1.32) | 0.2803 | C282Y variant | 1.70 (0.70–4.23) | 0.2409 |
| AgeAtDiagnosis | 1.00 (0.98–1.04) | 0.5381 | AgeAtDiagnosis | 1.00 (0.98–1.05) | 0.4285 |
| Tumor stage | 3.60 (1.93–6.55) | <0.0001 | Tumor stage | 4.20 (2.26–7.63) | <0.0001 |
| Smoking | 2.00 (1.08–3.55) | 0.0275 | Smoking | 1.90 (1.03–3.40) | 0.0392 |
| LUSC: | |||||
| H63D variant | 1.80 (0.59–5.24) | 0.3084 | C282Y variant | 0.32 (0.13–0.78) | 0.0130 |
| AgeAtDiagnosis | 1.00 (0.96–1.06) | 0.6639 | AgeAtDiagnosis | 1.00 (0.97–1.06) | 0.6231 |
| Tumor stage | 2.50 (1.10–5.68) | 0.0279 | Tumor stage | 2.40 (1.08–5.51) | 0.0316 |
| Smoking | 0.82 (0.36–1.84) | 0.6286 | Smoking | 0.58 (0.24–1.42) | 0.2349 |
LUAD (lung adenocarcinoma)
LUSC (lung squamous cell carcinoma)
HR (hazard ratio)
Covariates: Age at diagnosis (continuous), tumor stage (two categories, 3&4 vs 1&2), and smoking status (ever smoked vs never smoked)
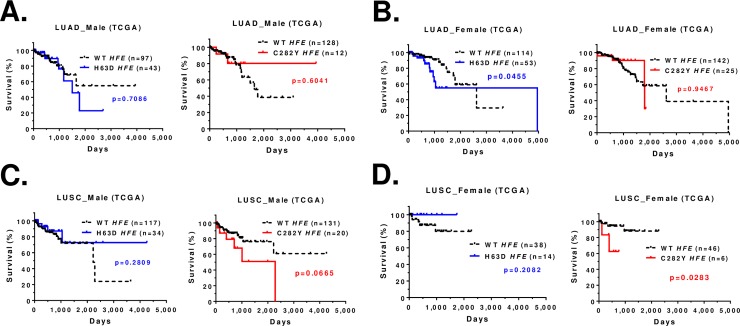
When we stratify the survival data by sex and HFE genotype we found that male LUAD patients with H63D HFE had no survival difference compared to WT HFE and female LUAD patients with H63D HFE had significantly poorer survival compared to WT HFE (p = 0.0455) (Fig 4A and 4B). The dramatic difference in survival for male LUSC patients with C282Y HFE compared to WT HFE did not reach statistical significance (p = 0.0665); however, female LUSC patients with C282Y HFE had significantly poorer survival compared to WT HFE (p = 0.0283) (Fig 4C and 4D).
Fig 4. Kaplan-Meier survival curve for TCGA lung cancer patients (Caucasians) based on sex and HFE genotype.
(A) Survival curve of male LUAD patients with WT or H63D HFE or C282Y HFE. (B) Survival curve of female LUAD patients with WT or H63D HFE or C282Y HFE. (C) Survival curve of male LUSC patients with WT or H63D HFE or C282Y HFE. (D) Survival curve of female LUSC patients with WT HFE or H63D HFE or C282Y HFE. Statistical analysis was performed by log-rank test and indicated as p value. Censored record is indicated as + in the graph.
We further compared the survival of lung cancer patients based on HFE expression and sex. The survival pattern was not different regardless of HFE expression levels in lung cancer patients. There were no survival differences between lower 50% and upper 50%, or between lower 25% and upper 75% in TCGA lung cancer dataset (S5 Fig). In general, the survival curve between males and females was not different regardless of HFE expression levels in lung cancer patients (S6 and S7 Figs). However, when HFE expression level is in the upper 50%, male LUAD and LUSC patients tend to had poorer survival than females (S6 and S7 Figs).
Discussion
The present study determined the frequency of HFE polymorphisms in lung cancer cell lines and human lung cancer patients. We found 7 of 10 lung cancer cell lines had the H63D or C282Y variant of the HFE gene. This result provided motivation to interrogate lung cancer samples from our institute and existing database such as TCGA for the frequency and impact of HFE gene variants on lung cancer.
There are significant HFE genotype and sex differences for survival and metastatic disease. In the TCGA lung cancer database, adenocarcinoma patients with H63D HFE trended to have poorer survival outcomes than WT HFE, but when the outcome data were stratified by sex the difference in survival outcome became statistically significant for females. The TCGA database does not include information on metastatic disease so we used our smaller internal database (PSHMC) and found a sex and genotype dependent effect for adenocarcinoma patients; males with the H63D HFE variant had less metastasis and females with the H63D HFE variant had more metastasis. There is no frequency increase in H63D HFE in the squamous cell cancer population or impact on the disease noted in our studies. These interesting results suggest that H63D HFE variant protects lung cancer metastasis in males, but enables metastasis in females. As far as we know, this is the first report for the impact of HFE variants and sex on lung cancer patients’ outcome.
In addition to the H63D variant of the HFE gene, the C282Y HFE variant is also found in the general population although at a lower prevalence. This gene variant has received considerable attention in hepatic cancers because of its tendency to be associated with hemochromatosis, the iron overload disease. In the TCGA database, individuals with squamous cell carcinoma that carry C282Y HFE have poorer survival than WT HFE. Moreover, when stratified for sex, it appears the females with C282Y are driving the significant difference as their survival outcome is much worse than males. There is no impact of this genotype of metastatic disease in the squamous cell cancer population. There is no statistically significant effect of C282Y HFE on the adenocarcinoma population, but there is a trend toward greater frequency of metastatic disease in males compared to females although the sample size is small. All these data suggest that females with C282Y HFE are a risk factor for lung squamous cell carcinoma. In our previous PSHMC GBM samples study, we found poorer survival in female metastatic brain tumor patients with C282Y HFE than WT HFE patients or male metastatic brain tumor patients with C282Y HFE [39]. The data implies that the metastatic potential of C282Y HFE is both cancer type and sex dependent.
Although we found HFE genotype and sex effect for lung cancer patient’s survival and metastatic disease, this is not related with the frequency of HFE genotype/alleles. For example, we observed higher frequency of C282Y HFE allele in female lung adenocarcinoma patients than male patients in TCGA; however, there was no survival difference between female C282Y HFE and male C282Y HFE lung adenocarcinoma patients. Instead, we found survival difference between female H63D HFE adenocarcinoma patients and female WT HFE adenocarcinoma patients.
In the present study, the level of HFE gene expression was not different between WT HFE and HFE variants of lung cancer patients (matched normal, primary tumors) in TCGA lung cancer data. In addition, HFE gene expression level did not impact survival of TCGA lung cancer patients (LUAD, LUSC) even when stratified for sex. These results suggest that poor survival in female lung adenocarcinoma with H63D HFE and female lung squamous cell cancer with C282Y HFE is not due to the expression level of HFE variants or frequency of HFE genotype but rather the function of HFE variant itself. There are many reports for the function of H63D or C282Y HFE in human cancer. For example, at the cellular level, the HFE H63D variant alters cholesterol metabolism [47], Endoplasmic Reticulum stress [48] and alters cancer phenotype [41, 49] including the protein profiles of exosomes [50]. Mouse H67D Hfe variant (human equivalent for H63D HFE variant) also alters macrophage function [51]. The C282Y HFE variant contributes therapy resistance and increased tumor burden [49]. Therefore, we will pursue the impact of sex and HFE variants in LUAD and LUSC in animal models as a future direction.
There are no consistent results between PSHMC and TCGA lung cancer samples for HFE genotype and cancer patient survival. When we compare the key variables between the TCGA lung cancer and the PSHMC samples, there are difference in age at diagnosis (e.g., median age: 70 years old for PSHMC vs. 67 years old for TCGA LUAD; p = 0.0026), smoking status (e.g., PSHMC vs. TCGA LUAD; p<0.0001), and the vital status (e.g., PSHMC vs. TCGA LUAD; p = 0.001) suggesting the PSHMC and TCGA cohorts have important distinctions. Therefore, we only showed Kaplan-Meier survival curve of PSHMC samples without Cox-regression results.
In summary, the H63D HFE gene variant is associated with poor survival and increased metastasis in female, but not male, LUAD patients. Although the frequency of C282Y HFE gene variant is higher in female LUAD patients than males, there was no gene effect on survival in these patients. However, the C282Y HFE gene variant is associated with poor survival in LUSC patients, especially females. The present findings indicate that there is a distinct impact of H63D and C282Y HFE variants in two different subtype of human lung cancers and impact of the genotype is influenced by sex.
Supporting information
(A) HFE gene expression based on WT HFE vs. H63D HFE in matched normal or primary tumor LUAD patients. (B) HFE gene expression based on WT HFE vs. C282Y HFE in matched normal or primary tumor LUAD patients. (C) HFE gene expression based on males vs. females in matched normal or primary tumor LUAD patients. P value was calculated from Wilcoxon rank sum tests to compare HFE expression values in the HFE mutant vs. HFE wild type.
(PPTX)
(A) HFE gene expression based on WT HFE vs. H63D HFE in matched normal or primary tumor LUSC patients. (B) HFE gene expression based on WT HFE vs. C282Y HFE in matched normal or primary tumor LUSC patients. (C) HFE gene expression based on males vs. females in matched normal or primary tumor LUSC patients. P value was calculated from Wilcoxon rank sum tests to compare HFE expression values in the HFE mutant vs. HFE wild type.
(PPTX)
(A) Survival curve of LUAD patients with WT HFE or H63D HFE. (B) Survival curve of LUAD patients with WT HFE or C282Y HFE. (C) Survival curve of LUSC patients with WT HFE or H63D HFE. (D) Survival curve of LUSC patients with WT HFE or C282Y HFE. Statistical analysis was performed by log-rank test and indicated as p value. Censored record is indicated as + in the graph.
(PPTX)
(A) Survival curve of LUAD patients with WT HFE or heterozygote or homozygote H63D HFE. (B) Survival curve of LUSC patients with WT HFE or heterozygote or homozygote C282Y HFE. LUSC with C282Y HFE heterozygote had poorer survival than WT HFE (p = 0.0052). Statistical analysis was performed by log-rank test and indicated as p value. Censored record is indicated as+ in the graph.
(PPTX)
(A) Kaplan-Meier survival curve of TCGA LUAD patients based on lower 50% or upper 50% of HFE gene expression. (B) Survival curve of TCGA LUAD patients between lower 25% and upper 75% of HFE gene expression. (C) Survival curve of TCGA LUSC patients based on lower 50% or upper 50% of HFE gene expression. (D) Survival curve of TCGA LUSC patients between lower 25% and upper 75% of HFE gene expression. P value was calculated from log rank tests to compare survival times in groups defined by HFE expression level.
(PPTX)
Survival curve between males and females of TCGA LUAD patients based on HFE gene expression at lower 25% (A) or lower 50% (B) or upper 50% (C) or upper 75% (D). Log rank tests were used to compare survival times in groups defined by HFE expression level.
(PPTX)
Survival curve between males and females of TCGA LUSC patients based on HFE gene expression at lower 25% (A) or lower 50% (B) or upper 50% (C) or upper 75% (D). Log rank tests were used to compare survival times in groups defined by HFE expression level.
(PPTX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank Penn State Institute for Personalized Medicine for providing the plasma samples of lung cancer patients. We also thank the macromolecular synthesis core and functional genomics core at the Penn State Health Milton S. Hershey Medical Center / Penn State Hershey College of Medicine for primer synthesis and DNA sequencing. We thank The Cancer Genome Atlas (TCGA) Data Access Committee. The results shown here are in whole or part based upon data generated by the TCGA Research Network (http://cancergenome.nih.gov). We thank Dr. Jong K. Yun for providing several lung cancer cell lines (H23, H441, H522, H838, H1299, and H1650). The authors thank Mrs. Sara Langan for critical editing.
Abbreviations
- ALK
Anaplastic lymphoma kinase
- ATCC
American Type Culture Collection
- EGFR
Epidermal growth factor receptor
- FGFR1
Fibroblast growth factor receptor 1
- GBM
glioblastoma
- KRAS
K-ras
- MHC
major histocompatibility complex
- LUAD
lung adenocarcinoma
- LUSC
lung squamous cell carcinoma
- NB
blood derived normal
- NSCLC
non-small cell lung cancer
- PSHMC
Penn State Hershey Medical Center
- PTEN
Phosphatase and tensin homolog
- RPMI
Roswell Park Memorial Institute
- SCLC
small cell lung cancer
- SLC11A1
Natural resistance-associated macrophage protein 1gene
- SNP
Single Nucleotide Polymorphism
- SNVs
Single Nucleotide Variants
- TCGA
The Cancer Genome Atlas
- TF
transferrin
- TFRC
transferrin receptor
- TP
primary solid tumor
- WT
wild type
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported in part by the Tara Leah Witmer Endowment. We would also like to acknowledge funding support from the Penn State Hershey Medical Center Dean’s Feasibility Grant (No grant number), Children’s Miracle Network (Penn State Hershey Medical Center), National Cancer Institute (Grant number 5 R21 CA167406-02), and Elsa U. Pardee Foundation (Grant number 138700, 125000). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Pennsylvania Department of Health and National Institutes of Health. There was no additional external funding received for this study.
References
- 1.American Cancer Society: Cancer Facts and Figures 2018. Atlanta, Ga: American Cancer Society, 2018. Available from: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2018.html [Google Scholar]
- 2.Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83(5): 584–594. 10.4065/83.5.584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zappa C, Mousa SA. Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res. 2016;5(3): 288–300. 10.21037/tlcr.2016.06.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ridge CA, McEriean AM, Ginsberg MS. Epidemiology of lung cancer. Semin Intervent Radiol. 2013;30(2): 93–98. 10.1055/s-0033-1342949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cook RM, Miller YE, Bunn PA Jr. Small cell lung cancer: etiology, biology, clinical features, staging, and treatment. Curr Probl Cancer. 1993;17(2): 69–141. 10.1016/0147-0272(93)90010-y [DOI] [PubMed] [Google Scholar]
- 6.Feng H, Wang X, Zhang Z, Tang C, Ye H, Jones L, et al. Identification of Genetic Mutations in Human Lung Cancer by Targeted Sequencing. Cancer Inform. 2015;14: 83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Telbany A, Ma PC. Cancer genes in lung cancer: racial disparities: are there any? Genes Cancer. 2012;3(7–8): 467–480. 10.1177/1947601912465177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lovly C, Horn L, Pao W. Molecular Profiling of Lung Cancer. My Cancer Genome (https://www.mycancergenome.org/content/disease/lung-cancer/). [Google Scholar]
- 9.Torti SV, Torti FM. Iron and cancer: more ore to be mined. Nat Rev Cancer. 2013;13(5): 342–355. 10.1038/nrc3495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang S, Chang W, Wu H, Wang YH, Gong YW, Zhao YL, et al. Pan-cancer analysis of iron metabolic landscape across the Cancer Genome Atlas. J Cell Physiol. 2019; 10.1002/jcp.29017 [DOI] [PubMed] [Google Scholar]
- 11.Pfeifhofer-Obermair C, Tymoszuk P, Petzer V, Weiss G, Nairz M. Iron in the Tumor Microenvironment-Connecting the Dots. Front Oncol. 2018;8: 549 10.3389/fonc.2018.00549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thielmann CM, Costa da Silva M, Muley T, Meister M, Herpel E, Muckenthaler MU. Iron accumulation in tumor-associated macrophages marks an improved overall survival in patients with lung adenocarcinoma. Sci Rep. 2019;9(1): 11326 10.1038/s41598-019-47833-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava A, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996;13(4): 399–408. 10.1038/ng0896-399 [DOI] [PubMed] [Google Scholar]
- 14.Gerhard GS, Paynton BV, DiStefano JK. Identification of Genes for Hereditary Hemochromatosis. Methods Mol Biol. 2018;1706: 353–365. 10.1007/978-1-4939-7471-9_19 [DOI] [PubMed] [Google Scholar]
- 15.Ali-Rahmani F, Schengrund CL, Connor JR. HFE gene variants, iron, and lipids: a novel connection in Alzheimer’s disease. Front Pharmacol. 2014;5: 165 10.3389/fphar.2014.00165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connor JR, Lee SY. Chapter 21. Iron and cancer In: Milner JA, Romagnolo DF, editors. Bioactive Compounds and Cancer; 2010. Humana/Springer Press; Pp. 469–496. [Google Scholar]
- 17.Chen J, Chloupkova M. Abnormal iron uptake and liver cancer. Cancer Biol Ther. 2009;8(18): 1699–1708. 10.4161/cbt.8.18.9146 [DOI] [PubMed] [Google Scholar]
- 18.Ellervik C, Birgens H, Tybjaerg-Hansen A, Nordestgaard BG. Hemochromatosis genotypes and risk of 31 disease endpoints: meta-analyses including 66,000 cases and 226,000 controls. Hepatology. 2007;46(4): 1071–1080. 10.1002/hep.21885 [DOI] [PubMed] [Google Scholar]
- 19.Hanson EH, Imperatore G, Burke W. HFE gene and hereditary hemochromatosis: a HuGE review, Human Genome Epidemiology. Am J Epidemiol. 2001;154(3): 193–206. 10.1093/aje/154.3.193 [DOI] [PubMed] [Google Scholar]
- 20.Adams PC, Reboussin DM, Barton JC, McLaren CE, Eckfeldt JH, McLaren GD, et al. Hemochromatosis and iron-overload screening in a racially diverse population. N Engl J Med. 2005;352(17): 1769–1778. 10.1056/NEJMoa041534 [DOI] [PubMed] [Google Scholar]
- 21.Steinberg KK, Cogswell ME, Chang JC, Caudill SP, McQuillian GM, Bowman BA, et al. Prevalence of C282Y and H63D mutations in the Hemochromatosis (HFE) gene in the United States. JAMA. 2001;285(17): 2216–2222. 10.1001/jama.285.17.2216 [DOI] [PubMed] [Google Scholar]
- 22.Viola A, Pagano L, Laudati D, D'Elia R, D'Amico MR, Ammirabile M, et al. HFE gene mutations in patients with acute leukemia. Leuk Lymphoma. 2006;47: 2331–2334. 10.1080/10428190600821898 [DOI] [PubMed] [Google Scholar]
- 23.Dorak MT, Burnett AK, Worwood M, Sproul AM, Gibson BE. The C282Y mutations of HFE is another male-specific risk factor for childhood acute lymphoblastic leukemia. Blood. 1999;94: 3957 [PubMed] [Google Scholar]
- 24.Gunel-Ozcan A, Alyilmaz-Bekmez S, Guler EN, Guc D. HFE H63D mutation frequency shows an increase in Turkish women with breast cancer. BMC Cancer. 2006;6: 37 10.1186/1471-2407-6-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu X, Lv C, Luan X, Lv M. C282Y polymorphism in the HFE gene is associated with risk of breast cancer. Tumour Biol. 2013;34(5): 2759–2764. 10.1007/s13277-013-0833-9 [DOI] [PubMed] [Google Scholar]
- 26.Martinez di Montemuros F, Tavazzi D, Salsano E, Piepoli T, Pollo B, Fiorelli G, Finocchiaro G. High frequency of the H63D mutation of the hemochromatosis gene (HFE) in malignant gliomas. Neurology. 2001;57: 1342. [DOI] [PubMed] [Google Scholar]
- 27.Shi Z, Johnstone D, Talseth-Palmer BA, Evans TJ, Spigelman AD, Groombridge C, et al. Haemochromatosis HFE gene polymorphisms as potential modifiers of hereditary nonpolyposis colorectal cancer risk and onset age. Int J Cancer. 2009;125: 78–83. 10.1002/ijc.24304 [DOI] [PubMed] [Google Scholar]
- 28.Ropero P, Briceño O, López-Alonso G, Agúndez JA, González Fernández FA, García-Hoz F, et al. The H63D mutation in the HFE gene is related to the risk of hepatocellular carcinoma. Rev Esp Enferm Dig. 2007;99: 376–381. 10.4321/s1130-01082007000700002 [DOI] [PubMed] [Google Scholar]
- 29.Shen LL, Gu DY, Zhao TT, Tang CJ, Xu Y, Chen JF. Implicating the H63D polymorphism in the HFE gene in increased incidence of solid cancers: a meta-analysis. Genet Mol Res. 2015;14(4): 13735–13745. 10.4238/2015.October.28.36 [DOI] [PubMed] [Google Scholar]
- 30.Ye Q, Qian BX, Yin WL, Wang FM, Han T. Association between the HFE C282Y, H63D Polymorphisms and the Risks of Non-Alcoholic Fatty Liver Disease, Liver Cirrhosis and Hepatocellular Carcinoma: An Updated Systematic Review and Meta-Analysis of 5,758 Cases and 14,741 Controls. PLoS One. 2016;11(9): e0163423 10.1371/journal.pone.0163423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang M, Xiong H, Fang L, Lu W, Wu X, Wang YQ, et al. Meta-Analysis of the Association between H63D and C282Y Polymorphisms in HFE and Cancer Risk. Asian Pac J Cancer Prev. 2015;16(11): 4633–4639. 10.7314/apjcp.2015.16.11.4633 [DOI] [PubMed] [Google Scholar]
- 32.Chen W, Zhao H, Li T, Yao H. HFE gene C282Y variant is associated with colorectal cancer in Caucasians: a meta-analysis. Tumour Biol. 2013;34(4): 2255–2259. 10.1007/s13277-013-0766-3 [DOI] [PubMed] [Google Scholar]
- 33.Jin F, Xiong WJ, Jing JC, Feng Z, Qu LS, Shen XZ. Evaluation of the association studies of single nucleotide polymorphisms and hepatocellular carcinoma: a systematic review. J Cancer Res Clin Oncol. 2011;137(7): 1095–1104. 10.1007/s00432-010-0970-0 [DOI] [PubMed] [Google Scholar]
- 34.Osborne NJ, Gurrin LC, Allen KJ, Constantine CC, Delatycki MB, McLaren CE, et al. HFE C282Y homozygotes are at increased risk of breast and colorectal cancer. Hepatology. 2010;51: 1311–1318. 10.1002/hep.23448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lv YF, Chang X, Hua RX, Yan GN, Meng G, Liao XY, et al. The risk of new-onset cancer associated with HFE C282Y and H63D mutations: evidence from 87,028 participants. J Cell Mol Med. 2016;20(7): 1219–1233. 10.1111/jcmm.12764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jin F, Qu LS, Shen XZ. Association between C282Y and H63D mutations of the HFE gene with hepatocellular carcinoma in European populations: a meta-analysis. J Exp Clin Cancer Res. 2010;29: 18 10.1186/1756-9966-29-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xiao-Bing H, Lu Z, Hong G, Ping L, Guanghui L, Hongming L, et al. Meta analysis on relationship between distributions of C282Y and H63D alleles and genotypes and hepatocellular carcinoma. Minerva Med. 2016. [Epub ahead of print] [PubMed] [Google Scholar]
- 38.Gannon PO, Medelci S, Le Page C, Beaulieu M, Provencher DM, Mes-Masson AM, et al. Impact of hemochromatosis gene (HFE) mutations on epithelial ovarian cancer risk and prognosis. Int J Cancer. 2011;128: 2326–2334. 10.1002/ijc.25577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee SY, Slagle-Webb B, Sheehan JM, Zhu J, Muscat JE, Glantz M, et al. HFE polymorphisms affect survival of brain tumor patients. J Neurooncol. 2015;122(1): 97–104. 10.1007/s11060-014-1681-1 [DOI] [PubMed] [Google Scholar]
- 40.Lee SY, Zhu J, Salzberg AC, Zhang B, Liu DJ, Muscat JE, et al. Analysis of single nucleotide variants of HFE gene and association to survival in The Cancer Genome Atlas GBM data. PLoS One. 2017;12(3): e0174778 10.1371/journal.pone.0174778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee SY, Patton SM, Henderson RJ, Connor JR. Consequences of expressing mutants of the hemochromatosis gene (HFE) into a human neuronal cell line lacking endogenous HFE. FASEB J. 2007;21(2): 564–576. 10.1096/fj.06-6397com [DOI] [PubMed] [Google Scholar]
- 42.Colaprico A, Silva TC, Olsen C, Garofano L, Cava C, Garolini D, et al. TCGAbiolinks: An R/Bioconductor package for integrative analysis of TCGA data. Nucleic Acids Res. 2016;44(8): e71 10.1093/nar/gkv1507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Silva CT, Colaprico A, Olsen C, D'Angelo F, Bontempi G, Ceccarelli M, et al. TCGA Workflow: Analyze cancer genomics and epigenomics data using Bioconductor packages. F1000Res. 2016;5: 1542 10.12688/f1000research.8923.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mounir M, Lucchetta M, Silva TC, Olsen C, Bontempi G, Chen X, et al. New functionalities in the TCGAbiolinks package for the study and integration of cancer data from GDC and GTEx. PLoS Comput Biol. 2019;15(3): e1006701 10.1371/journal.pcbi.1006701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.R Core Team. (2018) R: A language an environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria: https://www.R-project.org. [Google Scholar]
- 46.Therneau T. (2015) A package for survival analysis in S. version 2.38. https://CRAN.R-project.org/package=survival.
- 47.Ali-Rahmani F, Grigson PS, Lee S, Neely E, Connor JR, Schengrund CL. H63D mutation in hemochromatosis alters cholesterol metabolism and induces memory impairment. Neurobiol Aging. 2014;35(6): 1511.e1–12. [DOI] [PubMed] [Google Scholar]
- 48.Liu Y, Lee SY, Neely E, Nandar W, Moyo M, Simmons Z, et al. Mutant HFE H63D protein is associated with prolonged endoplasmic reticulum stress and increased neuronal vulnerability. J Biol Chem. 2011;286(15): 13161–13170. 10.1074/jbc.M110.170944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee SY, Liu S, Mitchell RM, Slagle-Webb B, Hong YS, Sheehan JM, et al. HFE polymorphisms influence the response to chemotherapeutic agents via induction of p16INK4A. Int J Cancer. 2011;129(9): 2104–2114. 10.1002/ijc.25888 [DOI] [PubMed] [Google Scholar]
- 50.Mrowczynski OD, Madhankumar AB, Slagle-Webb B, Lee SY, Zacharia BE, Connor JR. HFE genotype affects exosome phenotype in cancer. Biochim Biophys Acta Gen Subj. 2017;1861(8): 1921–1928. 10.1016/j.bbagen.2017.05.014 [DOI] [PubMed] [Google Scholar]
- 51.Nixon AM, Neely E, Simpson IA, Connor JR. The role of HFE genotype in macrophage phenotype. J Neuroinflammation. 2018;15(1): 30 10.1186/s12974-018-1057-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) HFE gene expression based on WT HFE vs. H63D HFE in matched normal or primary tumor LUAD patients. (B) HFE gene expression based on WT HFE vs. C282Y HFE in matched normal or primary tumor LUAD patients. (C) HFE gene expression based on males vs. females in matched normal or primary tumor LUAD patients. P value was calculated from Wilcoxon rank sum tests to compare HFE expression values in the HFE mutant vs. HFE wild type.
(PPTX)
(A) HFE gene expression based on WT HFE vs. H63D HFE in matched normal or primary tumor LUSC patients. (B) HFE gene expression based on WT HFE vs. C282Y HFE in matched normal or primary tumor LUSC patients. (C) HFE gene expression based on males vs. females in matched normal or primary tumor LUSC patients. P value was calculated from Wilcoxon rank sum tests to compare HFE expression values in the HFE mutant vs. HFE wild type.
(PPTX)
(A) Survival curve of LUAD patients with WT HFE or H63D HFE. (B) Survival curve of LUAD patients with WT HFE or C282Y HFE. (C) Survival curve of LUSC patients with WT HFE or H63D HFE. (D) Survival curve of LUSC patients with WT HFE or C282Y HFE. Statistical analysis was performed by log-rank test and indicated as p value. Censored record is indicated as + in the graph.
(PPTX)
(A) Survival curve of LUAD patients with WT HFE or heterozygote or homozygote H63D HFE. (B) Survival curve of LUSC patients with WT HFE or heterozygote or homozygote C282Y HFE. LUSC with C282Y HFE heterozygote had poorer survival than WT HFE (p = 0.0052). Statistical analysis was performed by log-rank test and indicated as p value. Censored record is indicated as+ in the graph.
(PPTX)
(A) Kaplan-Meier survival curve of TCGA LUAD patients based on lower 50% or upper 50% of HFE gene expression. (B) Survival curve of TCGA LUAD patients between lower 25% and upper 75% of HFE gene expression. (C) Survival curve of TCGA LUSC patients based on lower 50% or upper 50% of HFE gene expression. (D) Survival curve of TCGA LUSC patients between lower 25% and upper 75% of HFE gene expression. P value was calculated from log rank tests to compare survival times in groups defined by HFE expression level.
(PPTX)
Survival curve between males and females of TCGA LUAD patients based on HFE gene expression at lower 25% (A) or lower 50% (B) or upper 50% (C) or upper 75% (D). Log rank tests were used to compare survival times in groups defined by HFE expression level.
(PPTX)
Survival curve between males and females of TCGA LUSC patients based on HFE gene expression at lower 25% (A) or lower 50% (B) or upper 50% (C) or upper 75% (D). Log rank tests were used to compare survival times in groups defined by HFE expression level.
(PPTX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.